Maria Shepherd, President and Founder, Medi-Vantage10.08.19
No more call for physicians? Not really, but schedule predictability is in for physicians. Before healthcare reform, the archetypal interventionalist or surgeon had a private practice and was running a business where they could afford clinical/office staff to assist them. That has all been turned upside down for U.S. interventionalists, surgeons, and all other physicians as group practices have emerged, grown, and been transformed by employment contracts, practice management, and practice size changes. From 1996 to 2005, the percentage of physicians in single or two-physician practices dropped from 40.7 percent to 32.5 percent.1
Why This Is Important
The trend continues. Overall, the percentage of employed physicians is greater than self-employed physicians.2 Employed physicians (for example, hospital employees) were estimated in 2018 by a bi-annual AMA survey at 47.4 percent of all physicians involved in direct patient care. Self-employed physicians with ownership in a practice were estimated at 45.9 percent.2
As expected, physician ownership of practices differs when comparing specialties. Surgical medical specialties have the greatest share of ownership (estimated at 64.5 percent), and OBGYN practices follow at 53.8 percent.2 These data (Table 1) illustrate the ongoing trend of decreasing physician ownership of medical practices.
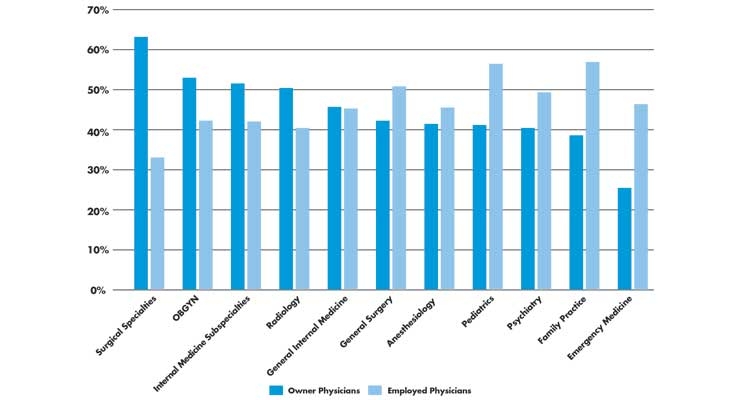
Table 1: Physician practice ownership vs. employed physicians (e.g., hospital employees) in 2018.2
It is reported that large group practices are more profitable because of resource-sharing, like practice managers and assistants. And, large practices have greater resources to negotiate with payers. But, an additional benefit of working for a hospital or large practice is the opportunity for greater work-life balance for doctors, because of the greater number of colleagues who can meet patient demand as proxies and share the burden of call for night and weekend work.3
Market Trends for Small Practices (under 10 physicians)
Most surprising was the finding that small physician practices (under 10 physicians; no longer one to two doctors) are still substantial. While the share of small practices has dropped consistently since 2012, 56.5 percent of physicians still worked in small practices in 2018—a drop of almost 5 percent as compared to 61.4 percent in 2012 (Table 2).2
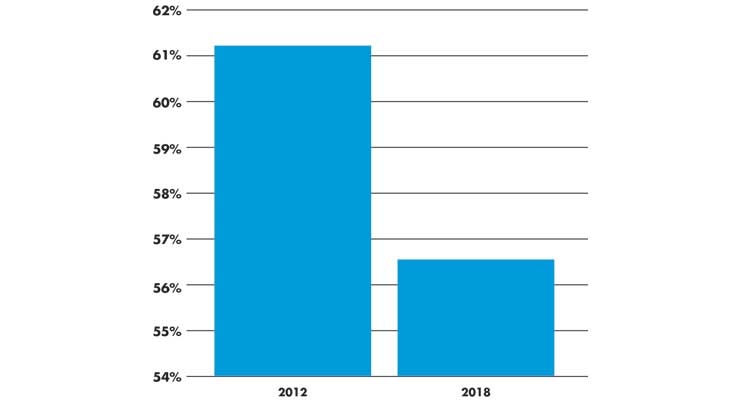
Table 2: The percentage of small physician practices (less than 10 physicians) in 2012 versus 2018.2
Further, medicine is emerging as a family-friendly business. In 2019, 70 percent of younger physicians (under 40 years old) reported being hospital employees and not practice owners. The majority of female doctors (of all ages) reported the same.3
Another emerging trend, the hospitalist, enables better hours for physicians. These are the medical specialists who see patients while they are hospitalized and manage in-patients based on directions from the physician specialists caring for them. Hospitalists help make doctors’ schedules predictable, because they work in shifts, reducing the need for call. Primary care physicians benefit enormously from the presence of hospitalists and don’t have to maintain a presence in the hospital (or over the phone) when their patients are admitted.3
However, the choice of medical specialty still varies by gender (Table 3) as female physicians often gravitate toward specialties that do not require as many hours.3
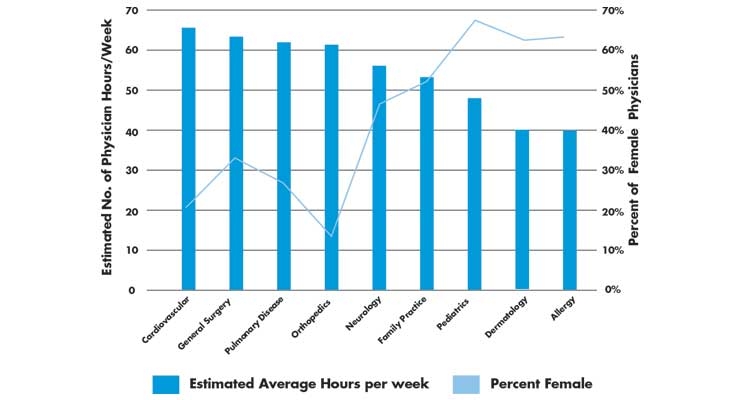
Table 3: View of physician specialty required estimated hours per week versus percentage of female physicians in the specialty.3
Hospitals Not the Only Buyers of Physician Practices
There is newly emerging competition for hospitals that plan to buy physician practices. Private equity (PE) groups are also investing in physician groups, and experts project that PE investment will continue.2,3 PE investors like domains that are fragmented and siloed. New physician practices need capital and PE is predicted to be a major participant in changing the healthcare market.4 Investments in all interventional or surgeon groups is being tracked as a major area of interest for PE.5
The Medi-Vantage Perspective
Physician ownership trends can affect medical device sales. Based on our research, physician-owned practices have a much greater sensitivity to the average sales price of medical devices in the context of reimbursement. We help our clients measure price sensitivity and assist them in developing validation tools to justify the cost of their devices. But, we expect escalating price sensitivity once PE firms become major investors in physician practices. PE firms are famous for taking profit by stripping out all the “fat” in an acquisition and with 18 to 20 percent of U.S. GDP spent in healthcare, there is plenty of low-lying fruit.
References
Maria Shepherd has more than 20 years of experience in medical device marketing in small startups and top-tier companies. After her industry career, including her role as VP of marketing for Oridion Medical, where she boosted the company valuation prior to its acquisition, director of marketing for Philips Medical, and senior management roles at Boston Scientific Corp., she founded Medi-Vantage. Medi-Vantage provides marketing, business strategy, and innovation research for the medical device, diagnostic, and digital health industries. The firm quantitatively and qualitatively sizes and segments opportunities, evaluates new technologies, provides marketing services, and assesses prospective acquisitions. Shepherd has taught marketing and product development courses and is a member of the Aligo Medtech Investment Committee (www.aligo.com). She can be reached at 855-343-3100. Visit her website at www.medi-vantage.com.
Why This Is Important
The trend continues. Overall, the percentage of employed physicians is greater than self-employed physicians.2 Employed physicians (for example, hospital employees) were estimated in 2018 by a bi-annual AMA survey at 47.4 percent of all physicians involved in direct patient care. Self-employed physicians with ownership in a practice were estimated at 45.9 percent.2
As expected, physician ownership of practices differs when comparing specialties. Surgical medical specialties have the greatest share of ownership (estimated at 64.5 percent), and OBGYN practices follow at 53.8 percent.2 These data (Table 1) illustrate the ongoing trend of decreasing physician ownership of medical practices.
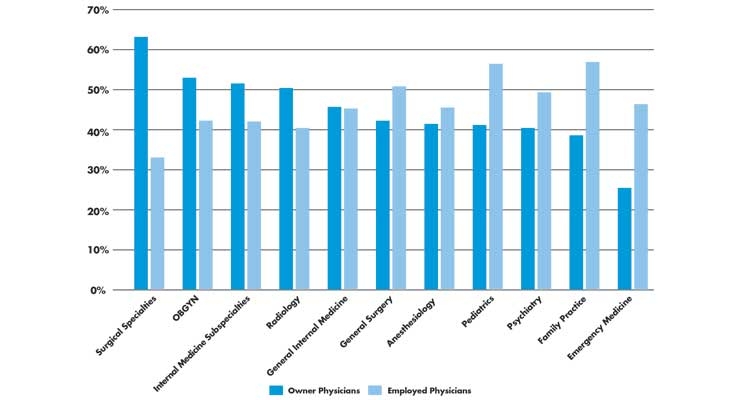
Table 1: Physician practice ownership vs. employed physicians (e.g., hospital employees) in 2018.2
It is reported that large group practices are more profitable because of resource-sharing, like practice managers and assistants. And, large practices have greater resources to negotiate with payers. But, an additional benefit of working for a hospital or large practice is the opportunity for greater work-life balance for doctors, because of the greater number of colleagues who can meet patient demand as proxies and share the burden of call for night and weekend work.3
Market Trends for Small Practices (under 10 physicians)
Most surprising was the finding that small physician practices (under 10 physicians; no longer one to two doctors) are still substantial. While the share of small practices has dropped consistently since 2012, 56.5 percent of physicians still worked in small practices in 2018—a drop of almost 5 percent as compared to 61.4 percent in 2012 (Table 2).2
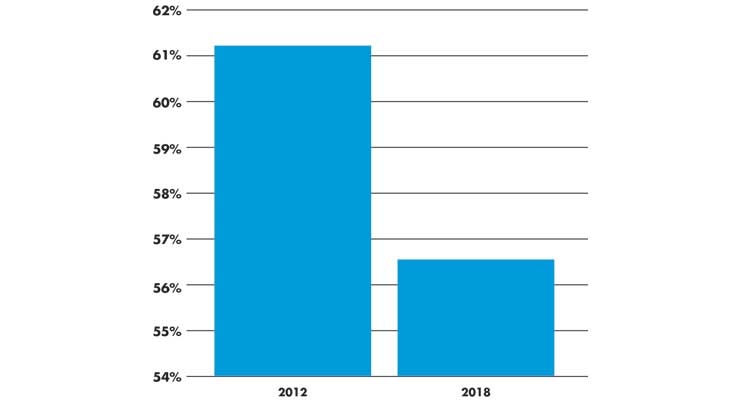
Table 2: The percentage of small physician practices (less than 10 physicians) in 2012 versus 2018.2
Further, medicine is emerging as a family-friendly business. In 2019, 70 percent of younger physicians (under 40 years old) reported being hospital employees and not practice owners. The majority of female doctors (of all ages) reported the same.3
Another emerging trend, the hospitalist, enables better hours for physicians. These are the medical specialists who see patients while they are hospitalized and manage in-patients based on directions from the physician specialists caring for them. Hospitalists help make doctors’ schedules predictable, because they work in shifts, reducing the need for call. Primary care physicians benefit enormously from the presence of hospitalists and don’t have to maintain a presence in the hospital (or over the phone) when their patients are admitted.3
However, the choice of medical specialty still varies by gender (Table 3) as female physicians often gravitate toward specialties that do not require as many hours.3
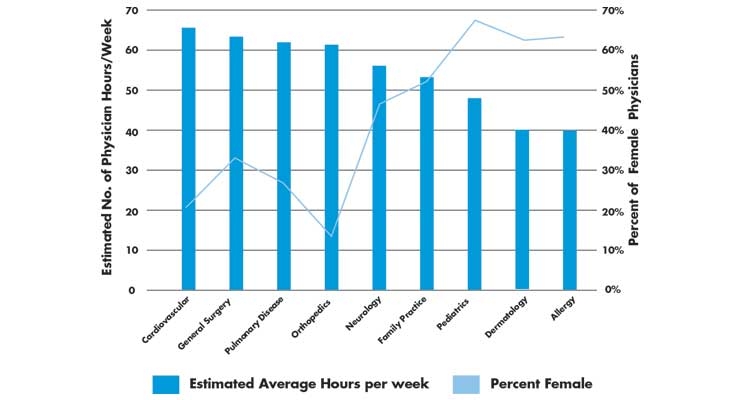
Table 3: View of physician specialty required estimated hours per week versus percentage of female physicians in the specialty.3
Hospitals Not the Only Buyers of Physician Practices
There is newly emerging competition for hospitals that plan to buy physician practices. Private equity (PE) groups are also investing in physician groups, and experts project that PE investment will continue.2,3 PE investors like domains that are fragmented and siloed. New physician practices need capital and PE is predicted to be a major participant in changing the healthcare market.4 Investments in all interventional or surgeon groups is being tracked as a major area of interest for PE.5
The Medi-Vantage Perspective
Physician ownership trends can affect medical device sales. Based on our research, physician-owned practices have a much greater sensitivity to the average sales price of medical devices in the context of reimbursement. We help our clients measure price sensitivity and assist them in developing validation tools to justify the cost of their devices. But, we expect escalating price sensitivity once PE firms become major investors in physician practices. PE firms are famous for taking profit by stripping out all the “fat” in an acquisition and with 18 to 20 percent of U.S. GDP spent in healthcare, there is plenty of low-lying fruit.
References
- http://bit.ly/mpo191001
- http://bit.ly/mpo191002
- http://bit.ly/mpo191003
- http://bit.ly/mpo191004
- http://bit.ly/mpo191005
Maria Shepherd has more than 20 years of experience in medical device marketing in small startups and top-tier companies. After her industry career, including her role as VP of marketing for Oridion Medical, where she boosted the company valuation prior to its acquisition, director of marketing for Philips Medical, and senior management roles at Boston Scientific Corp., she founded Medi-Vantage. Medi-Vantage provides marketing, business strategy, and innovation research for the medical device, diagnostic, and digital health industries. The firm quantitatively and qualitatively sizes and segments opportunities, evaluates new technologies, provides marketing services, and assesses prospective acquisitions. Shepherd has taught marketing and product development courses and is a member of the Aligo Medtech Investment Committee (www.aligo.com). She can be reached at 855-343-3100. Visit her website at www.medi-vantage.com.