Andrew Gaillard, Healthcare & Medical Segment Manager, Trelleborg Sealing Solutions12.05.19
There are two main categories of devices involving silicone combined with an active pharmaceutical ingredient. The first is liquid silicone rubber (LSR) combined with an API before being fabricated into a silicone part, usually part of a precise drug-delivery system. The second is a finished silicone part immersed in a drug- loaded solvent as a way to impregnate it with a drug, such as an antibacterial or antimicrobial.
With its stability and biocompatible properties, silicone is leading the way to a new generation of drug delivery products and enhanced medical devices that will profoundly improve patient care. In this article, we’ll look at the advantages, drawbacks, and manufacturing considerations of each process, along with examples of devices currently in use or development.
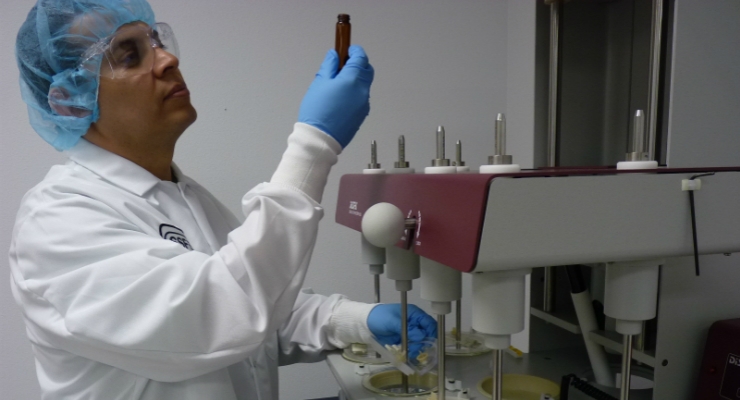
Drug Delivery: Adding an API to Raw Silicone
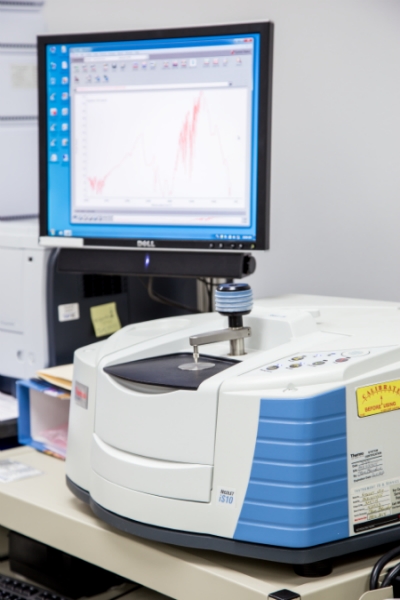
FTIR (Fourier Transform Infrared Spectroscopy) is used to determine the chemical composition of test samples. Image courtesy of Trelleborg Sealing Solutions.
The advantage of adding an API to silicone before fabrication is the ability to achieve an accurate mass ratio of drug to silicone. Typically, the ratio can be held to plus or minus 5% or better of the target mass ratio.
Thus, this process is ideal for creating devices designed to deliver a precise dose of medication, such as a skin patch for pain medication, a vaginal ring for contraception, or a bio-absorbable device for treating eye disease.
Most often, the API is combined with both the A and B sides of the silicone immediately before extrusion, molding, or sheeting. The API is usually added to the silicone in powder form, as this is typically the most stable form of the drug, but liquid formulations can be added.
There are several crucial manufacturing factors to consider when combining APIs with raw silicone. First, some APIs can poison the silicone cure. For example, chlorhexidine, a common antimicrobial, is available as a base and an acetate. If the acetate mixes and cures well with silicone, the base will poison the silicone cure.
Second, temperature plays a key role when adding APIs at this stage because the upper stability limit of many drugs is relatively low. For example, most hormones used in contraceptives begin to degrade at temperatures over 120 °C, but many silicone formulations have a cure temperature of 200°C. In this case, and many others, it’s important to select a low-temperature curing silicone and understand that the manufacturing process must be carefully controlled to ensure the temperature doesn’t exceed the stability limit of the drug.
Third, many APIs are hazardous in powdered form. For example, the amount of a micronized hormone that operating personnel can be subjected to is very small¾micrograms or even nanograms per day. Stringent engineering controls must be put in place and safety procedures carefully monitored.
Finally, all drug delivery products are subject to FDA or other regulatory body approval. So, whether the drug being delivered via the device is new or has already gained FDA approval, a full set of FDA trials (lab tests, animal tests, and human tests) are often required.
Device Enhancement: Impregnating Vulcanized Silicone with an API
There are several advantages to adding API to an existing silicone device through immersion: it’s a relatively mature technology, the timeline is usually short because the design/manufacturing process for the device doesn’t change, the bar is often lower for FDA approval, and the results are highly repeatable.
However, this process is not as precise as adding an API to raw silicone from a mass ratio perspective, so it’s only appropriate when precise drug-release rates aren’t critical. For example, the amount of anti-inflammatory released from a pacemaker lead does not need to be controlled in micrograms per day. Rather, the API is there to improve the safety or efficacy of the device, typically requiring a strong presence of the drug for the first two to four weeks after placement.
The process involves adding an API to a solvent that completely solubilizes the drug so the mixture is 100% homogenous. Common solvents for this application include chloroform, benzene, and toluene. The solvent swells the silicone, allowing the API to impregnate the vulcanized piece. After the immersion period, the component is removed from the solution and the solvent evaporates, leaving the API impregnated in the silicone matrix.
A number of variables, including the type of drug and the thickness of the materials, determine the amount of API that can be impregnated into the silicone. It’s important to work with a manufacturer familiar with the required development and testing procedures involved in determining the degree of impregnation.
Most often, APIs are added to some type of extruded material, such as a catheter or pacemaker lead, but this process works for calendared and molded components as well.
The main drawback of the immersion method for combination device production is the limited materials with which it will be successful. Silicone and some types of thermoplastic elastomers are essentially the most suitable materials.
Additionally, labeling for enhanced devices must be painstakingly considered. It’s difficult and time consuming to prove the efficacy of drug additives, although anecdotal evidence shows that adding antimicrobials usually reduces infection rates and anti-inflammatories have a positive effect on pacemaker lead performance. Many manufacturers are including drug additives in their device designs and simply claim that the addition may enhance performance or help prevent infection.
Indeed, the trend toward adding antimicrobials, anti-inflammatory drugs, or both to medical devices is quickly gaining traction in this industry segment. Allied Market Research published a report in September 2018 predicting that the global drug-device combination products market, which generated $81.3 billion in 2017, will reach $139.2 billion by 2025.
As implanted devices become a popular way to monitor chronic-disease patients (e.g., heart rate, glucose levels), guarding against inflammation and infection during and immediately following implantation is becoming key to successful outcomes. New devices, such as those that stimulate the nerves in the lower back to decrease pain, require a robust form of infection control to avoid introducing bacteria in the sensitive spinal area.
Andrew (Drew) Gaillard is the global director of the Healthcare and Medical Segment at Trelleborg Sealing Solutions. In this role, he is responsible for driving Trelleborg’s expertise in providing solutions to medical device and combination drug customers’ complex manufacturing challenges. Gaillard has held a variety of sales and marketing leadership roles throughout his career. He also has worked in international locations for a significant portion of that time. Prior to Trelleborg, Gaillard had his own strategic consulting business helping start-ups and small healthcare businesses determine go-to-market strategies. He was also the vice president of Global Marketing—Healthcare Division at Ecolab and spent 10 years in a variety of leadership roles in Medtronic’s cardiovascular group.
With its stability and biocompatible properties, silicone is leading the way to a new generation of drug delivery products and enhanced medical devices that will profoundly improve patient care. In this article, we’ll look at the advantages, drawbacks, and manufacturing considerations of each process, along with examples of devices currently in use or development.
Drug Delivery: Adding an API to Raw Silicone
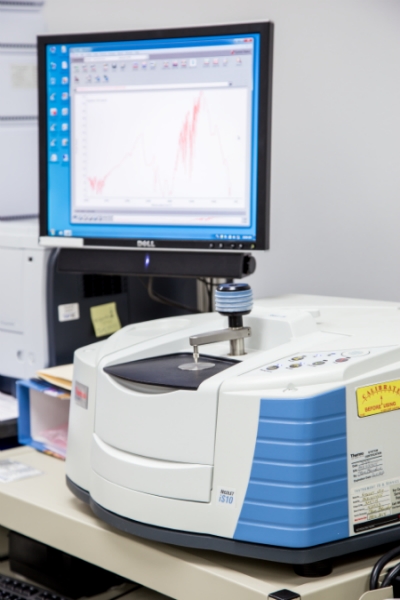
FTIR (Fourier Transform Infrared Spectroscopy) is used to determine the chemical composition of test samples. Image courtesy of Trelleborg Sealing Solutions.
The advantage of adding an API to silicone before fabrication is the ability to achieve an accurate mass ratio of drug to silicone. Typically, the ratio can be held to plus or minus 5% or better of the target mass ratio.
Thus, this process is ideal for creating devices designed to deliver a precise dose of medication, such as a skin patch for pain medication, a vaginal ring for contraception, or a bio-absorbable device for treating eye disease.
Most often, the API is combined with both the A and B sides of the silicone immediately before extrusion, molding, or sheeting. The API is usually added to the silicone in powder form, as this is typically the most stable form of the drug, but liquid formulations can be added.
There are several crucial manufacturing factors to consider when combining APIs with raw silicone. First, some APIs can poison the silicone cure. For example, chlorhexidine, a common antimicrobial, is available as a base and an acetate. If the acetate mixes and cures well with silicone, the base will poison the silicone cure.
Second, temperature plays a key role when adding APIs at this stage because the upper stability limit of many drugs is relatively low. For example, most hormones used in contraceptives begin to degrade at temperatures over 120 °C, but many silicone formulations have a cure temperature of 200°C. In this case, and many others, it’s important to select a low-temperature curing silicone and understand that the manufacturing process must be carefully controlled to ensure the temperature doesn’t exceed the stability limit of the drug.
Third, many APIs are hazardous in powdered form. For example, the amount of a micronized hormone that operating personnel can be subjected to is very small¾micrograms or even nanograms per day. Stringent engineering controls must be put in place and safety procedures carefully monitored.
Finally, all drug delivery products are subject to FDA or other regulatory body approval. So, whether the drug being delivered via the device is new or has already gained FDA approval, a full set of FDA trials (lab tests, animal tests, and human tests) are often required.
Device Enhancement: Impregnating Vulcanized Silicone with an API
There are several advantages to adding API to an existing silicone device through immersion: it’s a relatively mature technology, the timeline is usually short because the design/manufacturing process for the device doesn’t change, the bar is often lower for FDA approval, and the results are highly repeatable.
However, this process is not as precise as adding an API to raw silicone from a mass ratio perspective, so it’s only appropriate when precise drug-release rates aren’t critical. For example, the amount of anti-inflammatory released from a pacemaker lead does not need to be controlled in micrograms per day. Rather, the API is there to improve the safety or efficacy of the device, typically requiring a strong presence of the drug for the first two to four weeks after placement.
The process involves adding an API to a solvent that completely solubilizes the drug so the mixture is 100% homogenous. Common solvents for this application include chloroform, benzene, and toluene. The solvent swells the silicone, allowing the API to impregnate the vulcanized piece. After the immersion period, the component is removed from the solution and the solvent evaporates, leaving the API impregnated in the silicone matrix.
A number of variables, including the type of drug and the thickness of the materials, determine the amount of API that can be impregnated into the silicone. It’s important to work with a manufacturer familiar with the required development and testing procedures involved in determining the degree of impregnation.
Most often, APIs are added to some type of extruded material, such as a catheter or pacemaker lead, but this process works for calendared and molded components as well.
The main drawback of the immersion method for combination device production is the limited materials with which it will be successful. Silicone and some types of thermoplastic elastomers are essentially the most suitable materials.
Additionally, labeling for enhanced devices must be painstakingly considered. It’s difficult and time consuming to prove the efficacy of drug additives, although anecdotal evidence shows that adding antimicrobials usually reduces infection rates and anti-inflammatories have a positive effect on pacemaker lead performance. Many manufacturers are including drug additives in their device designs and simply claim that the addition may enhance performance or help prevent infection.
Indeed, the trend toward adding antimicrobials, anti-inflammatory drugs, or both to medical devices is quickly gaining traction in this industry segment. Allied Market Research published a report in September 2018 predicting that the global drug-device combination products market, which generated $81.3 billion in 2017, will reach $139.2 billion by 2025.
As implanted devices become a popular way to monitor chronic-disease patients (e.g., heart rate, glucose levels), guarding against inflammation and infection during and immediately following implantation is becoming key to successful outcomes. New devices, such as those that stimulate the nerves in the lower back to decrease pain, require a robust form of infection control to avoid introducing bacteria in the sensitive spinal area.
Andrew (Drew) Gaillard is the global director of the Healthcare and Medical Segment at Trelleborg Sealing Solutions. In this role, he is responsible for driving Trelleborg’s expertise in providing solutions to medical device and combination drug customers’ complex manufacturing challenges. Gaillard has held a variety of sales and marketing leadership roles throughout his career. He also has worked in international locations for a significant portion of that time. Prior to Trelleborg, Gaillard had his own strategic consulting business helping start-ups and small healthcare businesses determine go-to-market strategies. He was also the vice president of Global Marketing—Healthcare Division at Ecolab and spent 10 years in a variety of leadership roles in Medtronic’s cardiovascular group.