Maria Shepherd, President and Founder, Medi-Vantage03.07.19
It’s not called socialized medicine over here. The more radical proposal? A U.S. single-payer healthcare system called “Medicare for all.” Even former president Barack Obama, who long opposed a single-payer system for the United States, is backing the idea.1 “Democrats…are running on good new ideas like Medicare for all.”
In a Boston Globe article, journalists interviewed Sir Malcolm Grant, the former chairman of England’s National Health Service (NHS).1
There is big news from the NHS. In a recently announced long-term plan, several important objectives were made for the future of healthcare as supplied by Britain’s NHS. They state their single-payer system can also be a breeding ground for healthcare innovation. As Grant explained it, centralized policymaking combined with the data collection capabilities of the NHS are essential resources in developing and applying new technology.
Why This Is Important
Thinking of the NHS as a source of medical innovation is a doubtful concept to practitioners of U.S. medicine. Grant was prepared for disbelief on this side of the pond and noted that every healthcare system, globally, has high levels of waste. He believes much of the waste in the U.S. is a consequence of the multiple-payer system. Grant stated that, in the UK, they have dropped expenditures on administrative costs in the NHS to approximately 3.5 percent of total spend. In a recent New York Times article, the amount spent on administrative expenses in the U.S. was cited as 30 percent (Table 1).2
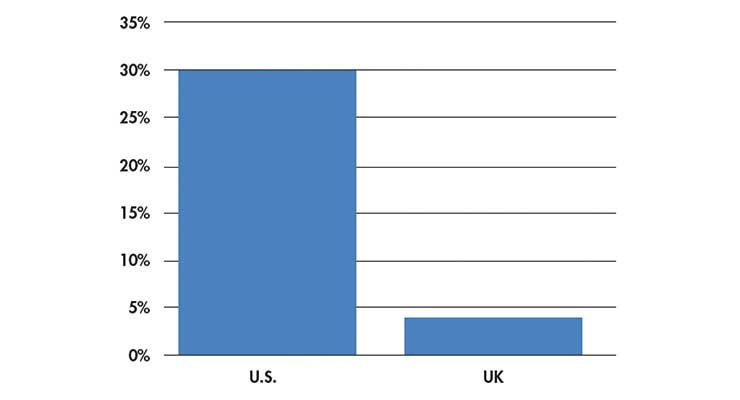
Table 1: Percent of healthcare expenditures resulting from administration.2
But doesn’t a single-payer system decrease choices for patients? Grant’s answer was that the possible cutback of choice is counterbalanced by the reduction of inequity. He stated that, in the UK, no person is impoverished by healthcare costs, ever.
The 800-Pound Gorilla in the Room—Crippling Healthcare Costs
We all know someone who has gone broke as a result of personal or a family member’s healthcare issues, whether it is the immense cost of a medication for Hepatitis C or progressive cancer care requiring treatments that can run over $100,000 and are not covered by private-payer insurance. In the NHS situation, the UK spreads financial risk across the entire community and recovers it in their progressive tax system.
According to the CDC, the average cost for just hospitalization associated with a coronary artery bypass surgery in the U.S. in 2013 was $38,707.3 In comparison, Table 2 offers a view of the average total costs for a coronary artery bypass surgical procedure (i.e., hospitalization and professional fees) in several countries. Note the U.S. cost comes in at $75,345. While the increase can be attributed to the inclusion of professional fees, the number is still substantial and administrative fees could be responsible for a significant portion of that difference.
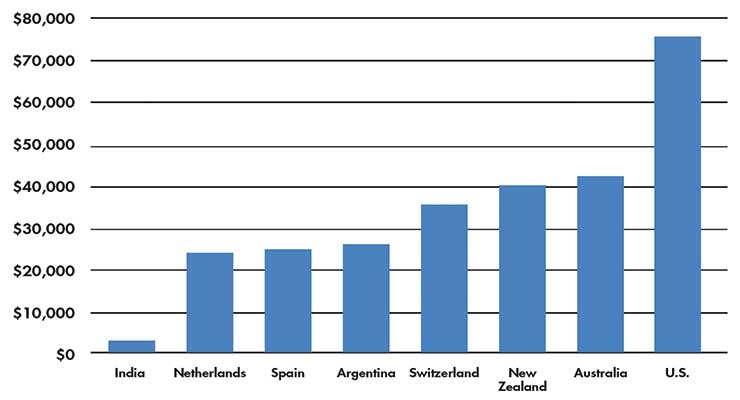
Table 2: Average total cost of a coronary artery bypass surgical procedure by country.3
Also revealed in Table 2 is the astonishingly low cost for a coronary artery bypass surgical procedure in India—$1,583. What type of quality of care is offered to these patients? It turns out, even at these very low costs, quality of care remains high according to Srinath Reddy, president of the Geneva-based World Heart Federation.4 These costs are the result of the efforts of a heart surgeon, Dr. Devi Shetty, who is also an entrepreneur and owns 21 medical centers in India. He cuts costs by turning off the air-conditioning, buying less expensive scrubs, and eliminating gratuitous pre-operative tests. In his facilities, the cost of a coronary artery bypass surgical procedure is now approximately $1,583, roughly 50 percent of the greater than $3,000 cost of the same procedure 20 years ago. Dr. Shetty wants to cut costs even further and expects to get the CABG procedure to approximately $800 over the next 10 years (Table 3).
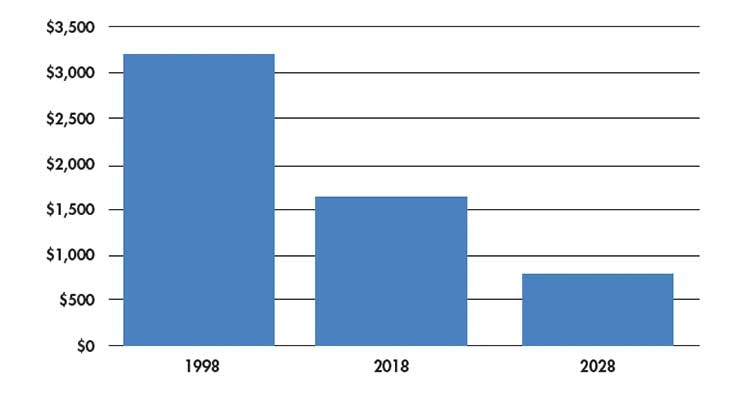
Table 3: Estimated past, current, and future costs for a coronary artery bypass surgical procedure in India.4
A word of warning to our electronic equipment medtech manufacturers. Dr. Shetty expects to gain some of these future cost reductions from Asian electronics medtech companies, as they launch new MRIs, CT scanners, and cath lab equipment.
The Medi-Vantage Perspective
Could the Indian business model work in the U.S.? Probably not, but a new NHS approach might. The NHS wants British patients to have the right to a digital-first consultation by 2024.
Grant believes much of the future of healthcare can be addressed through digital technology.1 Data is critical to this process. New changes at the NHS, plus an Uber-focused generation accustomed to digital access, could be the formula for success. For example, using FaceTime appointments with a general practitioner to get a prescription or to see if a diabetic wound is healing properly. The entire physician appointment can be retained in the cloud, and the patient can go back and look at it again, if necessary.
Grant knows primary care resources in the UK are limited. Patients must wait to see a general practitioner, who meets daily with an aging population with multiple comorbidities, which can’t be treated in 10-minute segments. A digital model that varies the workflow using a digital-first method could work, especially if reinforced by artificial intelligence (AI).
The difference AI could make is substantial. Grant referenced one of the models he has seen where, on the physician’s screen, the computer prompts him or her to, “Ask the patient about X, Y, and Z.” AI is able to determine the three most likely conditions afflicting the patient. Everyone wins. The physician is less fatigued by the high clinical case load, patients are getting questions relevant to their history and current symptoms, and the British healthcare system is treating a greater number of patients and experiencing more consistent outcomes.
References
Maria Shepherd has more than 20 years of leadership experience in medical device/life science marketing in small startups and top-tier companies. After her industry career, including her role as vice president of marketing for Oridion Medical, where she boosted the company valuation prior to its acquisition by Covidien/Medtronic, director of marketing for Philips Medical, and senior management roles at Boston Scientific Corp., she founded Medi-Vantage. Medi-Vantage provides marketing, business strategy, and innovation research for the medical device, diagnostic, and digital health industries. The firm quantitatively and qualitatively sizes and segments opportunities, evaluates new technologies, provides marketing services, and assesses prospective acquisitions. Shepherd has taught marketing and product development courses and is a member of the Aligo Medtech Investment Committee (www.aligo.com). She can be reached at 855-343-3100. Visit her website at www.medi-vantage.com.
In a Boston Globe article, journalists interviewed Sir Malcolm Grant, the former chairman of England’s National Health Service (NHS).1
There is big news from the NHS. In a recently announced long-term plan, several important objectives were made for the future of healthcare as supplied by Britain’s NHS. They state their single-payer system can also be a breeding ground for healthcare innovation. As Grant explained it, centralized policymaking combined with the data collection capabilities of the NHS are essential resources in developing and applying new technology.
Why This Is Important
Thinking of the NHS as a source of medical innovation is a doubtful concept to practitioners of U.S. medicine. Grant was prepared for disbelief on this side of the pond and noted that every healthcare system, globally, has high levels of waste. He believes much of the waste in the U.S. is a consequence of the multiple-payer system. Grant stated that, in the UK, they have dropped expenditures on administrative costs in the NHS to approximately 3.5 percent of total spend. In a recent New York Times article, the amount spent on administrative expenses in the U.S. was cited as 30 percent (Table 1).2
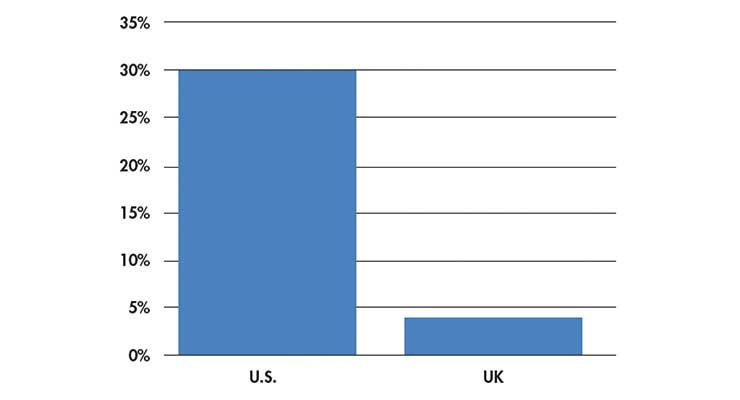
Table 1: Percent of healthcare expenditures resulting from administration.2
But doesn’t a single-payer system decrease choices for patients? Grant’s answer was that the possible cutback of choice is counterbalanced by the reduction of inequity. He stated that, in the UK, no person is impoverished by healthcare costs, ever.
The 800-Pound Gorilla in the Room—Crippling Healthcare Costs
We all know someone who has gone broke as a result of personal or a family member’s healthcare issues, whether it is the immense cost of a medication for Hepatitis C or progressive cancer care requiring treatments that can run over $100,000 and are not covered by private-payer insurance. In the NHS situation, the UK spreads financial risk across the entire community and recovers it in their progressive tax system.
According to the CDC, the average cost for just hospitalization associated with a coronary artery bypass surgery in the U.S. in 2013 was $38,707.3 In comparison, Table 2 offers a view of the average total costs for a coronary artery bypass surgical procedure (i.e., hospitalization and professional fees) in several countries. Note the U.S. cost comes in at $75,345. While the increase can be attributed to the inclusion of professional fees, the number is still substantial and administrative fees could be responsible for a significant portion of that difference.
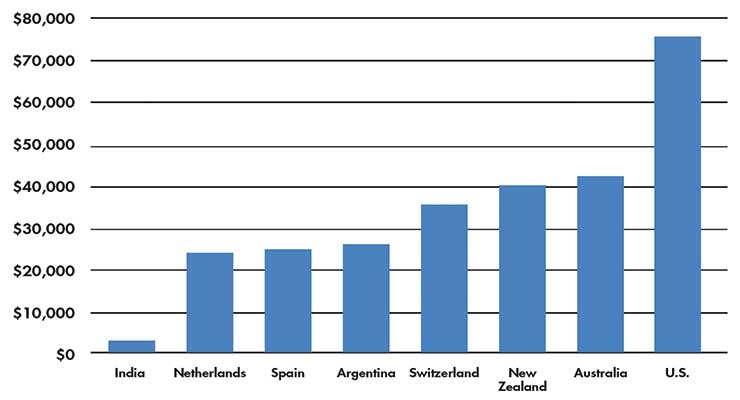
Table 2: Average total cost of a coronary artery bypass surgical procedure by country.3
Also revealed in Table 2 is the astonishingly low cost for a coronary artery bypass surgical procedure in India—$1,583. What type of quality of care is offered to these patients? It turns out, even at these very low costs, quality of care remains high according to Srinath Reddy, president of the Geneva-based World Heart Federation.4 These costs are the result of the efforts of a heart surgeon, Dr. Devi Shetty, who is also an entrepreneur and owns 21 medical centers in India. He cuts costs by turning off the air-conditioning, buying less expensive scrubs, and eliminating gratuitous pre-operative tests. In his facilities, the cost of a coronary artery bypass surgical procedure is now approximately $1,583, roughly 50 percent of the greater than $3,000 cost of the same procedure 20 years ago. Dr. Shetty wants to cut costs even further and expects to get the CABG procedure to approximately $800 over the next 10 years (Table 3).
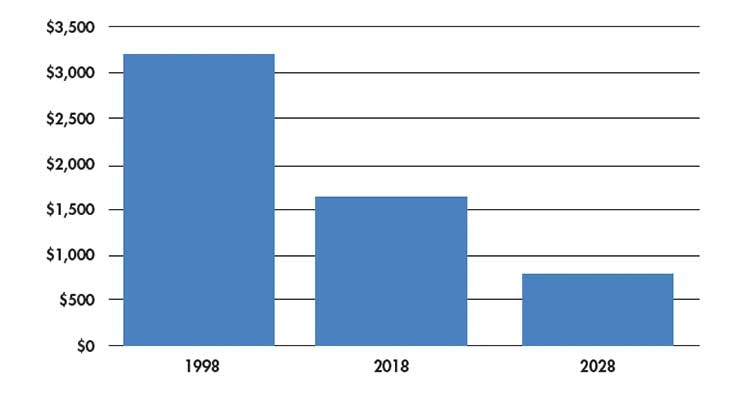
Table 3: Estimated past, current, and future costs for a coronary artery bypass surgical procedure in India.4
A word of warning to our electronic equipment medtech manufacturers. Dr. Shetty expects to gain some of these future cost reductions from Asian electronics medtech companies, as they launch new MRIs, CT scanners, and cath lab equipment.
The Medi-Vantage Perspective
Could the Indian business model work in the U.S.? Probably not, but a new NHS approach might. The NHS wants British patients to have the right to a digital-first consultation by 2024.
Grant believes much of the future of healthcare can be addressed through digital technology.1 Data is critical to this process. New changes at the NHS, plus an Uber-focused generation accustomed to digital access, could be the formula for success. For example, using FaceTime appointments with a general practitioner to get a prescription or to see if a diabetic wound is healing properly. The entire physician appointment can be retained in the cloud, and the patient can go back and look at it again, if necessary.
Grant knows primary care resources in the UK are limited. Patients must wait to see a general practitioner, who meets daily with an aging population with multiple comorbidities, which can’t be treated in 10-minute segments. A digital model that varies the workflow using a digital-first method could work, especially if reinforced by artificial intelligence (AI).
The difference AI could make is substantial. Grant referenced one of the models he has seen where, on the physician’s screen, the computer prompts him or her to, “Ask the patient about X, Y, and Z.” AI is able to determine the three most likely conditions afflicting the patient. Everyone wins. The physician is less fatigued by the high clinical case load, patients are getting questions relevant to their history and current symptoms, and the British healthcare system is treating a greater number of patients and experiencing more consistent outcomes.
References
Maria Shepherd has more than 20 years of leadership experience in medical device/life science marketing in small startups and top-tier companies. After her industry career, including her role as vice president of marketing for Oridion Medical, where she boosted the company valuation prior to its acquisition by Covidien/Medtronic, director of marketing for Philips Medical, and senior management roles at Boston Scientific Corp., she founded Medi-Vantage. Medi-Vantage provides marketing, business strategy, and innovation research for the medical device, diagnostic, and digital health industries. The firm quantitatively and qualitatively sizes and segments opportunities, evaluates new technologies, provides marketing services, and assesses prospective acquisitions. Shepherd has taught marketing and product development courses and is a member of the Aligo Medtech Investment Committee (www.aligo.com). She can be reached at 855-343-3100. Visit her website at www.medi-vantage.com.