Dr. Andreas Alt, Sales Director—Medical, Sensirion03.01.19
Inhalers are among the most commonly used devices for treating respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD). With each inhalation through the inhaler, the device delivers a specific amount of medication to the lungs. However, when it comes to proper inhaler use, misuse is the norm.
It is well documented that patients often have problems adopting the correct inhaler technique, and thus, receive insufficient medication. This applies equally to both metered dose inhalers (MDIs) and dry powder inhalers (DPIs), and leads to poor disease control and increased healthcare costs either as a result of uncontrolled disease, increased drug utilization for relief medication, preventative therapy, or emergency department visits. This remains a common problem in both asthma and COPD.1,2
Global annual costs associated with asthma and COPD management is substantial from both the healthcare payer and the societal perspective. Research findings show that healthcare spending for an uncontrolled patient is more than double that of a controlled patient.3
Studies have also found that patients make at least one mistake during inhaler drug intake as often as 70 percent to 90 percent of the time, resulting in only 7 percent to 40 percent of the drug being delivered to the lungs.4 The two biggest and most serious errors when using an MDI are both related to patient inhalation. The first error is related to the coordination between inhalation and triggering the dose release of the inhaler. Even a short delay can result in only 20 percent of the medication being delivered to the lungs.4 The second most significant error is not breathing deeply enough, which can cause another 10 percent less medication to reach the lungs.4
The opportunity for technological innovation to reduce these common errors by measuring patient inhalation airflow through the inhaler device is already available today and allows for increased drug delivery efficacy, improved medication adherence, reduced healthcare costs and, ultimately, improved patient outcomes.
Why Measure the Inhalation Flow Profile?
As discussed previously, the two biggest and most serious errors in using inhalers are related to patient inhalation. By measuring the inhaled airflow through the inhaler, and additionally registering the point in time when the drug is dispensed for MDIs, allows information on whether the drug was released within the optimal window of the inhalation cycle to be accurately determined (Figure 1). This dose-trigger timing versus flow correlation is one critical parameter to understanding if the drug carrying flow reached deep into the bronchia and achieved the desired high lung deposition (Figure 2).
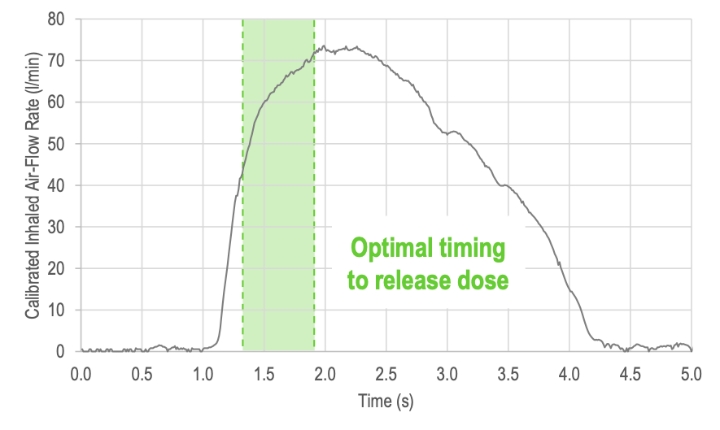
Figure 1: Inhalation flow profile showing the calibrated flow rate in standard liters per minute (l/min) versus the inhalation time in seconds (s).
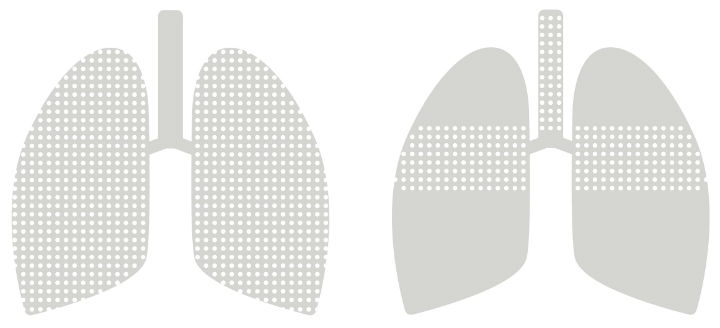
Figure 2: Schematic illustration of drug deposition when the drug is released in the optimal timing window (left side) and when the drug is released too late (right side).
The second critical parameter is the inhaled airflow profile. Borrowing from spirometry, several parameters can be derived from the inhalation airflow profile that provide insights into each patient’s inhalation:
Accurate and calibrated real-time recordings of the inhalation flow profile provide the information above, from which it can be determined whether the patient carried out the inhalation correctly and achieved a high lung deposition during inhalation. Other parameters of interest include the inspired vital capacity (IVC) and peak inspired flow rate (PIF), along with the full inhalation airflow characteristic as shown in Figure 3.
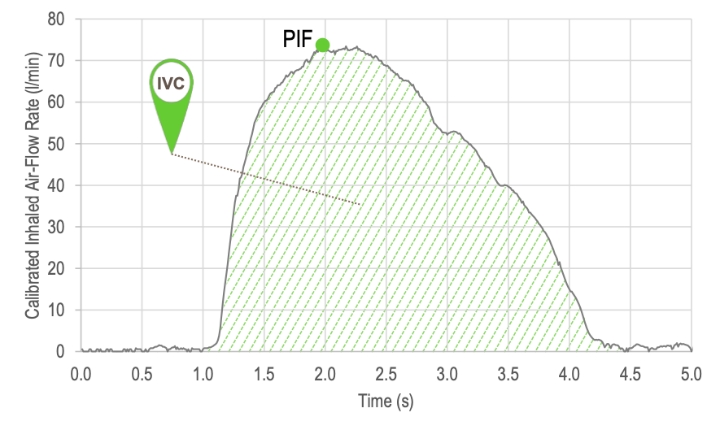
Figure 3: Parameters derived from the inhalation airflow characteristic: inspired vital capacity (IVC) and peak inspired flow rate (PIF).
Subsets of parameters such as forced inspired volume during the first second of inhalation (FIV1) or the airway resistance (RAW) can also be determined from the inhalation airflow profile. The derivation of the latter is shown in Figure 4.
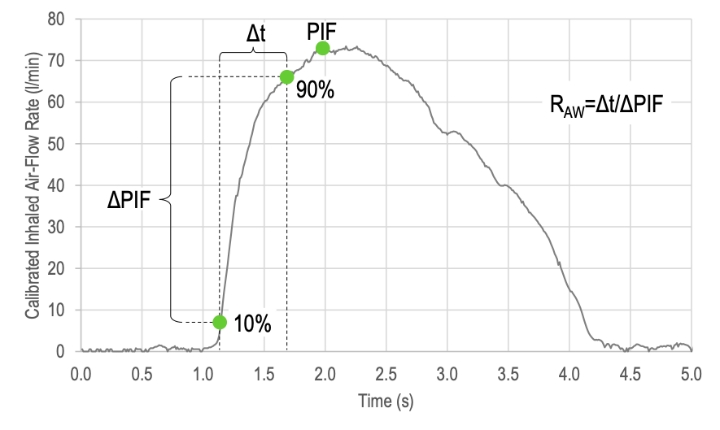
Figure 4: Besides the peak inspired airflow (PIF), the airway resistance (RAW) can be determined from calibrated inhalation airflow characteristics recorded with a sufficient high temporal and flow resolution.
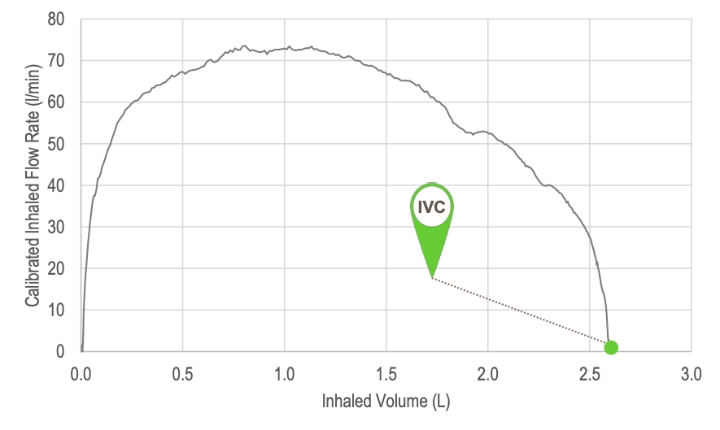
Figure 5: Typical spirometer plot of flow rate versus inhaled volume. The inspired vital capacity (IVC) is the total inhaled volume as the flow rate returns to zero at the end of the inhalation.
Some parameters such as airway resistance (RAW) can be of special interest for patients with COPD as it may relate directly to the condition of the disease. As the inhaler is now being utilized as a spirometer-like device, all parameters are derived upon use of the inhaler without any additional effort or time-related burden to the patient. Besides monitoring every inhalation through the inhaler for its quality and the correct use of the inhaler, the above parameters monitored over time can additionally provide feedback on the effectiveness of the medication, the course of the disease and alert the healthcare professional or be motivational for the patient and increase adherence.
Cohero Health already provides patients with an additional spirometer for exactly this reason (i.e., to allow the patients to routinely measure their lung function over the course of the treatment). The benefit of providing direct disease management and sharing this data with medical professionals helps patients and clinicians to assess treatment progress and also enables payment-by-results rather than pay-per-dose. This same development can be observed in the insulin or sleep apnea industry where it has led to growing market shares for companies offering connected devices in recent years and simultaneously brought down treatment costs and improved patient outcomes. Most importantly, this combination of drug delivery and diagnostic unit in a single device is a powerful tool in improving patient outcomes.
Figure 6 shows the schematic behavior of PIF, IVC, and RAW versus time. It visualizes the positive effect of starting the treatment, the stable treatment phase during regular dosage, and the negative effect of interrupting the treatment.

Figure 6: Peak inspired airflow (PIF), inspired vital capacity (IVC) and airway resistance (RAW) monitored over time, providing valuable feedback to the healthcare professional and the patient.
By adding the capability of measuring flow to the drug delivery inhaler device, not only can patient compliance and correct use of the inhaler be monitored, but also the effectiveness of the medication and course of the disease over time can be observed by utilizing the spirometer-like lung function recordings.
Next generation inhalers—natively incorporating airflow measurements in their design—will facilitate automatic dose release at the optimal point in time, individually tailored to the patient and their specific condition.
How to Measure the Inhalation Flow Profile
Before inhalers natively include electronics and connectivity features by design, existing inhalers and inhaler platforms can be enhanced with the required electronics to achieve connectivity and the required sensing functionality. This is already being done today by companies such as Propeller Health, Adherium, and others that have designed a variety of clip-ons for existing inhalers to add connectivity by monitoring parameters such as date and time of usage as well as evaluating signals from additional sensors such as accelerometers, GPS and many more. In the past, accurate measurement of the flow through the inhaler was challenging due to the lack of sufficiently robust and yet sensitive devices capable of measuring the smallest flows. In order to avoid revalidation of the inhaler with the FDA and maintain approval, the key regulatory requirement for all inhaler clip-ons demands that the flow path of the inhaler remains unaltered in order to ensure that it does not interfere with the existing inhaler device function.
In order to demonstrate how accurate flow measurement through an inhaler can be realized without interfering with the flow path, a functional inhaler clip-on has been developed by Sensirion. Figure 7 shows the 3D-printed inhaler clip-on containing the Sensirion flow sensor SDP3x as well as a Bluetooth low energy communications chip and a battery power source. It is notable that the inhaler housing has not been altered in any way and the flow measurement principle relies solely on the Venturi/Bernoulli principle at the inhaler inlet. The calibrated inhaler airflow shows excellent agreement to an external flow reference and was used for obtaining the flow profiles depicted in this article.

Figure 7: 3D-printed inhaler clip-on containing the Sensirion flow sensor SDP3x in the side view (left) and top view (right) showing the unobstructed flow path of the inhaler.
The unaltered and unobstructed inhaler flow path design is enabled by the extreme sensitivity of the Sensirion MEMS-based (micro electro mechanical system) flow chip solution utilized in the SDP3x flow sensor series. This technology is based on the microthermal flow-through principle, the next generation hotwire flow sensor technology that has been successfully used in medical ventilators for decades. In clip-ons for existing inhalers as well as newly developed inhalers, the key advantages of Sensirion’s CMOSens flow chip technology can be summarized as:
Outlook of Flow Measurement in Smart Inhalers
Adding a diagnostic unit to the drug delivery device that the patient is already familiar with is a powerful tool in asthma and COPD disease management. Improper inhalation technique leads to decreased efficacy through reduced deposition of drug in the lungs, which in turn leads to increasing disease severity and thus a worse patient outcome and an increase in healthcare costs. The solution of guiding the patient and providing direct feedback as well as supporting the patient in controlling the disease and increasing adherence have already been shown to improve patient outcomes by current connected drug delivery devices.
Thus, robust and accurate flow measurement is an important feature towards better disease management and patient outcomes and is already realizable today. The high percentage of patients suffering from asthma or COPD and misusing their inhaler when a life free of complaints would generally be possible with proper disease management will continue to drive innovation for connected drug delivery. An increasing number of companies are implementing digital technologies in their products already today to provide an enhanced method of managing asthma and COPD as well as improving the effectiveness of medication. Supporting the patient with the optimal treatment of their disease, not solely as a simple medical tool but as a companion device to remind, coach and provide relevant insight into the treatment and the course of the disease, is the direction in which the industry is advancing.
References
1 A. Melani, M. Bonavia, V. Cilenti, C. Cinti, M. Lodi, P. Martucci and et al., "Inhaler mishandling remains common in real life and is associated with reduced disease control," Respir Med, vol. 105, no. 6, pp. 930-938, June 2011.
2 V. Press, V. Arora, L. Shah, S. Lewis, K. Ivy, J. Charbeneau and et al., "Misuse of respiratory inhalers in hospitalized patients with asthma or COPD," J Gen Intern Med, vol. 26, no. 6, pp. 635-642, June 2011.
3 S. Sullivan, "The burden of uncontrolled asthma on the US health care system," Managed Care, vol. 14, no. 8, pp. 4-7, 2005.
4 R. Biswas, N. A. Hanania and A. Sabharwal, "Factors Determining In Vitro Lung Deposition of Albuterol Aerosol Delivered by Ventolin Metered-Dose Inhaler," Journal of Aerosol Medicine and Pulmonary Drug Delivery, vol. 30, no. 4, August 2017.
Dr. Andreas Alt is sales director medical at Sensirion. He leads Sensirion’s medical business and oversees the worldwide expansion of sensors and sensor solutions for the measurement and control of flow and environmental parameters into medical devices. Furthermore, Dr. Alt is responsible for medical OEM projects. He has a Ph.D. in electrical engineering and experience in strategic market development and international project management.
It is well documented that patients often have problems adopting the correct inhaler technique, and thus, receive insufficient medication. This applies equally to both metered dose inhalers (MDIs) and dry powder inhalers (DPIs), and leads to poor disease control and increased healthcare costs either as a result of uncontrolled disease, increased drug utilization for relief medication, preventative therapy, or emergency department visits. This remains a common problem in both asthma and COPD.1,2
Global annual costs associated with asthma and COPD management is substantial from both the healthcare payer and the societal perspective. Research findings show that healthcare spending for an uncontrolled patient is more than double that of a controlled patient.3
Studies have also found that patients make at least one mistake during inhaler drug intake as often as 70 percent to 90 percent of the time, resulting in only 7 percent to 40 percent of the drug being delivered to the lungs.4 The two biggest and most serious errors when using an MDI are both related to patient inhalation. The first error is related to the coordination between inhalation and triggering the dose release of the inhaler. Even a short delay can result in only 20 percent of the medication being delivered to the lungs.4 The second most significant error is not breathing deeply enough, which can cause another 10 percent less medication to reach the lungs.4
The opportunity for technological innovation to reduce these common errors by measuring patient inhalation airflow through the inhaler device is already available today and allows for increased drug delivery efficacy, improved medication adherence, reduced healthcare costs and, ultimately, improved patient outcomes.
Why Measure the Inhalation Flow Profile?
As discussed previously, the two biggest and most serious errors in using inhalers are related to patient inhalation. By measuring the inhaled airflow through the inhaler, and additionally registering the point in time when the drug is dispensed for MDIs, allows information on whether the drug was released within the optimal window of the inhalation cycle to be accurately determined (Figure 1). This dose-trigger timing versus flow correlation is one critical parameter to understanding if the drug carrying flow reached deep into the bronchia and achieved the desired high lung deposition (Figure 2).
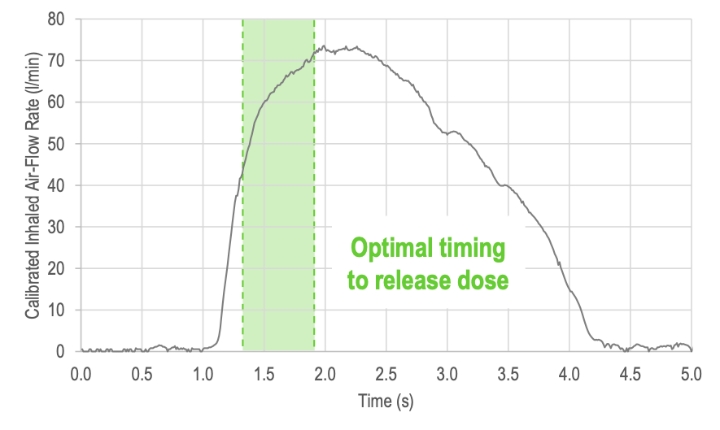
Figure 1: Inhalation flow profile showing the calibrated flow rate in standard liters per minute (l/min) versus the inhalation time in seconds (s).
Figure 2: Schematic illustration of drug deposition when the drug is released in the optimal timing window (left side) and when the drug is released too late (right side).
The second critical parameter is the inhaled airflow profile. Borrowing from spirometry, several parameters can be derived from the inhalation airflow profile that provide insights into each patient’s inhalation:
- Depth and length of inhalation
- Entire exhalation before inhaling
- Slow inhalation according to instructions
- Lung function and its development over time
Accurate and calibrated real-time recordings of the inhalation flow profile provide the information above, from which it can be determined whether the patient carried out the inhalation correctly and achieved a high lung deposition during inhalation. Other parameters of interest include the inspired vital capacity (IVC) and peak inspired flow rate (PIF), along with the full inhalation airflow characteristic as shown in Figure 3.
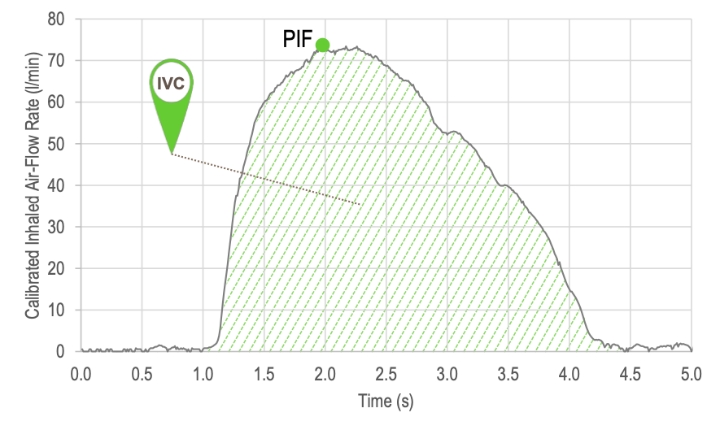
Figure 3: Parameters derived from the inhalation airflow characteristic: inspired vital capacity (IVC) and peak inspired flow rate (PIF).
Subsets of parameters such as forced inspired volume during the first second of inhalation (FIV1) or the airway resistance (RAW) can also be determined from the inhalation airflow profile. The derivation of the latter is shown in Figure 4.
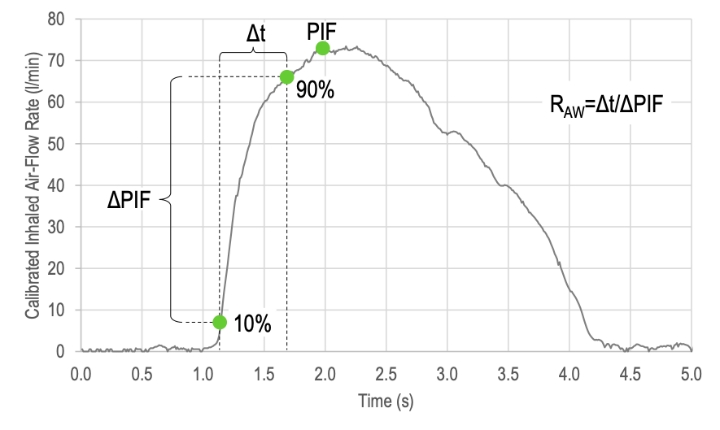
Figure 4: Besides the peak inspired airflow (PIF), the airway resistance (RAW) can be determined from calibrated inhalation airflow characteristics recorded with a sufficient high temporal and flow resolution.
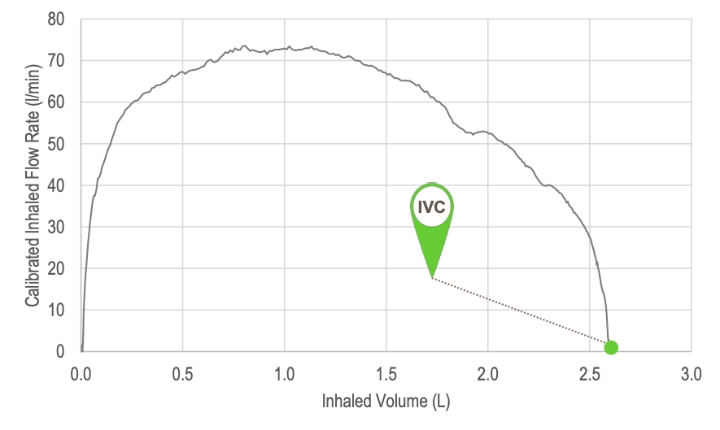
Figure 5: Typical spirometer plot of flow rate versus inhaled volume. The inspired vital capacity (IVC) is the total inhaled volume as the flow rate returns to zero at the end of the inhalation.
Some parameters such as airway resistance (RAW) can be of special interest for patients with COPD as it may relate directly to the condition of the disease. As the inhaler is now being utilized as a spirometer-like device, all parameters are derived upon use of the inhaler without any additional effort or time-related burden to the patient. Besides monitoring every inhalation through the inhaler for its quality and the correct use of the inhaler, the above parameters monitored over time can additionally provide feedback on the effectiveness of the medication, the course of the disease and alert the healthcare professional or be motivational for the patient and increase adherence.
Cohero Health already provides patients with an additional spirometer for exactly this reason (i.e., to allow the patients to routinely measure their lung function over the course of the treatment). The benefit of providing direct disease management and sharing this data with medical professionals helps patients and clinicians to assess treatment progress and also enables payment-by-results rather than pay-per-dose. This same development can be observed in the insulin or sleep apnea industry where it has led to growing market shares for companies offering connected devices in recent years and simultaneously brought down treatment costs and improved patient outcomes. Most importantly, this combination of drug delivery and diagnostic unit in a single device is a powerful tool in improving patient outcomes.
Figure 6 shows the schematic behavior of PIF, IVC, and RAW versus time. It visualizes the positive effect of starting the treatment, the stable treatment phase during regular dosage, and the negative effect of interrupting the treatment.

Figure 6: Peak inspired airflow (PIF), inspired vital capacity (IVC) and airway resistance (RAW) monitored over time, providing valuable feedback to the healthcare professional and the patient.
By adding the capability of measuring flow to the drug delivery inhaler device, not only can patient compliance and correct use of the inhaler be monitored, but also the effectiveness of the medication and course of the disease over time can be observed by utilizing the spirometer-like lung function recordings.
Next generation inhalers—natively incorporating airflow measurements in their design—will facilitate automatic dose release at the optimal point in time, individually tailored to the patient and their specific condition.
How to Measure the Inhalation Flow Profile
Before inhalers natively include electronics and connectivity features by design, existing inhalers and inhaler platforms can be enhanced with the required electronics to achieve connectivity and the required sensing functionality. This is already being done today by companies such as Propeller Health, Adherium, and others that have designed a variety of clip-ons for existing inhalers to add connectivity by monitoring parameters such as date and time of usage as well as evaluating signals from additional sensors such as accelerometers, GPS and many more. In the past, accurate measurement of the flow through the inhaler was challenging due to the lack of sufficiently robust and yet sensitive devices capable of measuring the smallest flows. In order to avoid revalidation of the inhaler with the FDA and maintain approval, the key regulatory requirement for all inhaler clip-ons demands that the flow path of the inhaler remains unaltered in order to ensure that it does not interfere with the existing inhaler device function.
In order to demonstrate how accurate flow measurement through an inhaler can be realized without interfering with the flow path, a functional inhaler clip-on has been developed by Sensirion. Figure 7 shows the 3D-printed inhaler clip-on containing the Sensirion flow sensor SDP3x as well as a Bluetooth low energy communications chip and a battery power source. It is notable that the inhaler housing has not been altered in any way and the flow measurement principle relies solely on the Venturi/Bernoulli principle at the inhaler inlet. The calibrated inhaler airflow shows excellent agreement to an external flow reference and was used for obtaining the flow profiles depicted in this article.

Figure 7: 3D-printed inhaler clip-on containing the Sensirion flow sensor SDP3x in the side view (left) and top view (right) showing the unobstructed flow path of the inhaler.
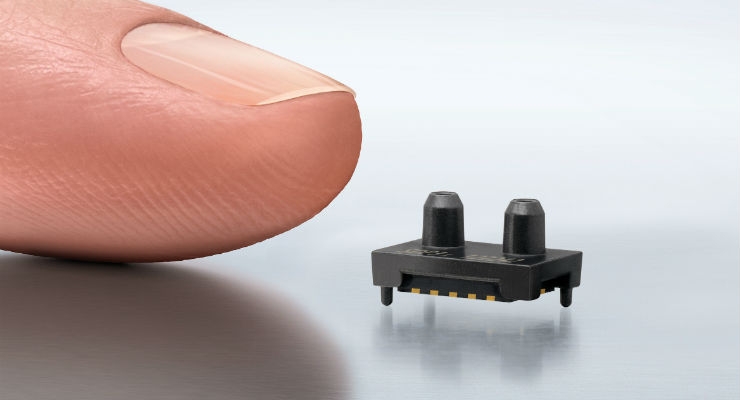
The unaltered and unobstructed inhaler flow path design is enabled by the extreme sensitivity of the Sensirion MEMS-based (micro electro mechanical system) flow chip solution utilized in the SDP3x flow sensor series. This technology is based on the microthermal flow-through principle, the next generation hotwire flow sensor technology that has been successfully used in medical ventilators for decades. In clip-ons for existing inhalers as well as newly developed inhalers, the key advantages of Sensirion’s CMOSens flow chip technology can be summarized as:
- Highest sensitivity down to hundredths of a Pascal
- High temporal and pressure/flow accuracy
- Proven device in the medical and automotive industry
- Robust against being dropped and ultra-sonic welding process steps
- Inherently robust against external disturbances by the two-port design
- Low power consumption for portable and battery operation
- World’s smallest commercially available flow sensor
Outlook of Flow Measurement in Smart Inhalers
Adding a diagnostic unit to the drug delivery device that the patient is already familiar with is a powerful tool in asthma and COPD disease management. Improper inhalation technique leads to decreased efficacy through reduced deposition of drug in the lungs, which in turn leads to increasing disease severity and thus a worse patient outcome and an increase in healthcare costs. The solution of guiding the patient and providing direct feedback as well as supporting the patient in controlling the disease and increasing adherence have already been shown to improve patient outcomes by current connected drug delivery devices.
Thus, robust and accurate flow measurement is an important feature towards better disease management and patient outcomes and is already realizable today. The high percentage of patients suffering from asthma or COPD and misusing their inhaler when a life free of complaints would generally be possible with proper disease management will continue to drive innovation for connected drug delivery. An increasing number of companies are implementing digital technologies in their products already today to provide an enhanced method of managing asthma and COPD as well as improving the effectiveness of medication. Supporting the patient with the optimal treatment of their disease, not solely as a simple medical tool but as a companion device to remind, coach and provide relevant insight into the treatment and the course of the disease, is the direction in which the industry is advancing.
References
1 A. Melani, M. Bonavia, V. Cilenti, C. Cinti, M. Lodi, P. Martucci and et al., "Inhaler mishandling remains common in real life and is associated with reduced disease control," Respir Med, vol. 105, no. 6, pp. 930-938, June 2011.
2 V. Press, V. Arora, L. Shah, S. Lewis, K. Ivy, J. Charbeneau and et al., "Misuse of respiratory inhalers in hospitalized patients with asthma or COPD," J Gen Intern Med, vol. 26, no. 6, pp. 635-642, June 2011.
3 S. Sullivan, "The burden of uncontrolled asthma on the US health care system," Managed Care, vol. 14, no. 8, pp. 4-7, 2005.
4 R. Biswas, N. A. Hanania and A. Sabharwal, "Factors Determining In Vitro Lung Deposition of Albuterol Aerosol Delivered by Ventolin Metered-Dose Inhaler," Journal of Aerosol Medicine and Pulmonary Drug Delivery, vol. 30, no. 4, August 2017.
Dr. Andreas Alt is sales director medical at Sensirion. He leads Sensirion’s medical business and oversees the worldwide expansion of sensors and sensor solutions for the measurement and control of flow and environmental parameters into medical devices. Furthermore, Dr. Alt is responsible for medical OEM projects. He has a Ph.D. in electrical engineering and experience in strategic market development and international project management.