The (Virtual) Doctor Is In (via Telemedicine)
By Sam Brusco, Associate Editor | 06.04.20
Virtual healthcare delivery is flourishing due to the COVID-19 pandemic, but will it persist once the crisis has subsided?
On May 20, Eko, a firm that develops technology to detect and monitor cardiac and respiratory disease by bringing together advanced sensors, patient and provider software, and AI-powered analysis, announced what the company claims to be the first and only AI-powered telehealth platform for virtual cardiac and pulmonary monitoring. Eko Telehealth combines stethoscope and single-lead ECG live-streaming combined with embedded HIPAA-compliant video conferencing and FDA-cleared algorithms to spot heart murmurs and AFib.
“Video telemedicine and virtual patient visits only go so far. Patients with complex cardiovascular diseases will receive incomplete care through just video conference. It’s critical that a provider is able to assess a patient’s heart and lung function remotely,” Eko CEO and co-founder Connor Landgraf told the press. “The Eko intelligent telehealth platform gives providers the most comprehensive picture of a patient’s heart and lung health. Virtual cardiac and pulmonary medicine will become the standard of care even after the pandemic abates.”
Using this technology, providers at hospitals, rural clinics, or nursing homes can stream stethoscope audio and ECG readings to a physician in another room or at a virtual care center, medical center, or specialty clinic. Patients can operate the stethoscope under the supervision of a healthcare provider and use a mobile application to connect via video conference with providers to navigate a self-operated cardiac and pulmonary exam.
Eko Telehealth is one of the latest innovations in telehealth (or telemedicine), the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status. Telehealth encompasses a rising number of applications and technologies including two-way live or streaming video, videoconferencing, store-and-forward imaging along with the internet, e-mail, smartphones, wireless tools, and other forms of telecommunication. These technologies facilitate leverage of the latest advancements in computer, network, and peripheral medical equipment to promote health. Telehealth is considered to be an integral component of processes that will align with the future of healthcare and improve outcomes in all areas of medicine.
“Innovation in new connected devices and the ability to transmit biometric data in real-time to increase the diagnostic capabilities of the virtual consultations have allowed telehealth capabilities to expand beyond traditional observational consultations,” said S. John Korangy, M.D., founder and CEO of CareClix Inc., an Alexandria, Va.-based provider of software and services for telemedicine and virtual health.
Web Real-Time Communication (WebRTC), a standard to connect two or more users in a private, secure video connection using only a web browser, was designed by Google and open sourced in 2011. Major internet products like Facebook, Google Hangouts, Amazon Kindle, and Slack have used WebRTC technology to build video into applications for customer support or social interaction.
A standard WebRTC application connects two or more users in a Peer-to-Peer (P2P) connection through a Signaling Server custom built for the application. Once the connection is established, the users are connected to each other in a private encrypted connection, allowing them to directly share video, audio, and data with each other. No intermediary servers are required for this, making the connection very secure.
“WebRTC (Web Real-Time Communication)-based solutions built into modern web browsers represent the greatest innovation for telehealth capabilities,” said Jordan Rosen, CEO of Lille Group, an Albany, N.Y.-based provider of healthcare software and technology solutions that improve patient care, reduce costs, and enable healthcare professionals to work most effectively. “Google Chrome has the most complete support; Mozilla Firefox is a very close second. Apple's Safari is significantly behind the other browsers, but the Jitsi community is working hard to close the gap.”
Ease-of-use is of the utmost importance when designing a telehealth platform. The technology has to be accessible to everyone from the most tech-savvy of Millennials to elderly patients that struggle with newer technologies. There must be a simple interface and minimal software installation required to create a platform that can be widely adopted.
“It’s important to first understand the target audience and prioritize the patient experience,” said Charlie Mason, SVP of strategic accounts at Sanmina, a San Jose, Calif.-headquartered global contract manufacturing firm. “If a chronically ill and elderly patient must use a home device to log certain health parameters that are remotely communicated to a doctor, it must be simple and straightforward to use. Highly sophisticated devices may work well in a hospital or doctor’s office, but if they are not intuitive with simple displays, large buttons, and built-in cellular connectivity, they may not be adopted by home users.”
“The portability and durability of a device and an understanding of how it will be used in the home setting, such as in a bathroom or kitchen, are also important considerations to factor into the product development plan,” he added.
“The challenge is to ensure the patient doesn’t have to be a technical guru to join a video call,” said Rosen. “A WebRTC-based solution requires no additional software to install—calls are initiated from the web browser. If you are limited to running Safari, particularly on a smartphone, download the Jitsi Meet app. We delivered a robust telehealth solution in a matter of several days by combining SMS messaging (via Twilio) to invite patients to the virtual appointment with the simplicity of browser-based access.”
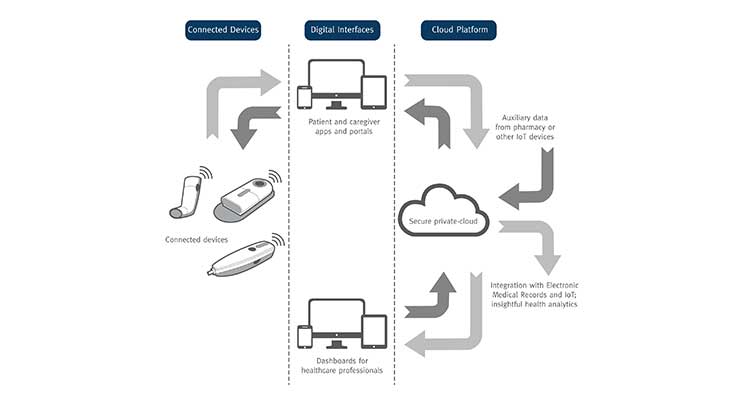
Connectivity technology is one of the most efficient ways to gather patient data and offer instructional content for patients, healthcare providers, caregivers, and payers. To use a telehealth platform to increase patient medication adherence and outcomes of therapies, a 360-degree focus must be placed on patients, caregivers, and healthcare providers. A well-functioning, reliable connected health system that embraces all aspects of digital health is necessary to accomplish this.
Partnering with a specialized firm on a connected health system allows collection and analysis of patient data related to diagnosis and medication adherence. Patients can be motivated and instructed on treatment information and medication administration.
“The latest innovations are two-fold: reduced cost and complexity of connectivity and simple sensors, and an increased portion of the population with smartphones and other technologies that facilitate healthcare provider-patient engagement and disease self-management,” said Bill Welch, chief technology officer of Hudson, Wis.-based Phillips-Medisize (a Molex company), a technology-based, global outsource provider of design and manufacturing services, with significant business in the drug delivery, medical device, and primary pharmaceutical packaging markets. “We have designed our low-cost connectivity module to further reduce the cost of creating and manufacturing connected devices by use of a common architecture.”
The COVID-19 pandemic has transformed the delivery of healthcare seemingly overnight. As healthcare institutions attempt to implement social distancing and triage patients, virtual visits with doctors have skyrocketed. According to the Wall Street Journal, CMS telehealth visits surged from 100,000 a week to 300,000 a week as of March 28, and the agency expects this to increase.
"I think the genie's out of the bottle on this one," CMS administrator Seema Verma told Becker’s Hospital Review. "I think it's fair to say that the advent of telehealth has been just completely accelerated, that it’s taken this crisis to push us to a new frontier, but there's absolutely no going back."
Telehealth service providers have rushed to fulfill the sudden need for innovation in their programs the pandemic has created.
“We have been offering our services very much in line with our prior existing programs,” said Dr. Korangy. “We have been adding more laboratory testing partnerships to address the COVID-19 pandemic, as lab testing is a key component.”
“We quickly developed/integrated a telemedicine video conferencing component (Jitsi Meet) to call and access patients within a short time frame for our eScribeHost EHR platform for cardiology users,” added Dennis Vetrano, R.N., director of sales and business development at Lille Group.
Lille Group’s Cardiac Signals cloud-based software solution automatically incorporates transmissions from major cardiac implant device manufacturers (including Medtronic, Boston Scientific, BIOTRONIK, and Abbott Laboratories) into one HHS/CMS certified platform to easily manage a population of patients enrolled in remote monitoring. The platform simplifies management of transmissions while automatically capturing and identifying all billable events.
“We released the Cardiac Signals cloud-based solution to manage remote cardiac implant patients, who need to be remotely monitored. All their transmissions need review by cardiologists or ANP,” said Vetrano. “Cardiology practice ‘Device or Pacer Clinics’ were essentially shut down to most implant patients due to COVID-19—there is a high risk of major complications and morbidity if these patients are infected. Cardiac Signals allows cardiology practices to efficiently manage more device patients and their transmissions, triage appropriately, and capture all billing while providing quality care remotely to Heart Rhythm Society Class I standards.”
Home-based diagnostic testing has become an especially important aspect of telehealth due to the pandemic because patients don’t have to risk exposure from a trip to a testing site to collect a sample. On April 21, the FDA re-issued emergency use authorization for LabCorp’s COVID-19 RT-PCR test to allow testing of samples self-collected by patients at home using the company’s home collection kit. Further, the FDA authorized the first COVID-19 diagnostic test using at-home collection of saliva specimens for emergency use on May 8, to Rutgers Clinical Genomics Laboratory.
“There is a unique opportunity to make home-based testing for infectious diseases more prevalent due to the COVID-19 pandemic and the desire for rapid ongoing testing that can be performed while maintaining social distancing guidelines,” said Mason. “This enabling technology could significantly change how we identify illnesses by reducing the amount of time and number of in-person interactions required to get a diagnosis. If parents suspect their child might be sick with the flu, they could either use a home test system ordered online or pick one up at a pharmacy, avoiding further exposure by visiting a doctor’s office or a lab. We’re currently engaged with a number of companies exploring this business model.”
Connected drug delivery devices are also increasingly being developed to support patient supervision and counseling in the home setting. These advanced devices include features like dosing reminders, adherence trackers, educational tools, and patient diaries to collect patient-reported outcomes. They may also include monitoring tools with interfaces between patients and healthcare professionals.
“There has been significant growth in diagnostics, including devices with the potential for connectivity to track infectious disease data by patient location.,” said Welch. “Our embedded software, hardware design, and electronics manufacturing capabilities are all growing. We support COVID-19 in many categories, from hospital equipment to patient drug delivery devices that allow self-administration vs. going to a healthcare provider for administration. Some of our customers’ innovative drug inhalation devices are also being evaluated for use with direct-to-lung medications to treat COVID-19 respiratory issues.”
Barriers to Adoption
So what’s standing in the way of a proliferation of telehealth services becoming the “new normal”?
“Hospitals have been very slow to upgrade/change their server-based systems to cloud-based systems,” said Vetrano. “The COVID-19 pandemic has sent a loud and clear message to upgrade IT systems to provide quality care, improve efficiency with all staff touching the patient remotely, reduce IT cost and labor, and generate new value-based revenue—especially with chronically ill patients at high risk of serious complications if infected with COVID-19. These patients will need to remain away from the hospital environment unless a clinical intervention is necessary.”
Unfortunately, hospital sluggishness is just one of the many barriers to widespread telehealth adoption. There’s still confusion about what services will and won’t be reimbursed. Costs associated with implementing a telemedicine program can include a great deal of factors like video conferencing adoption and remote monitoring expansion. Healthcare security breaches are on the rise, and patient data can be exposed. Providers may also encounter patient reluctance to engage virtually despite proper broadband and internet resources.
“Connectivity is still an issue in certain parts of the country,” said Dr. Korangy. “Certain patient populations also don’t have the technical capabilities to take full advantage of telehealth.”
A number of other barriers have slowed the widespread adoption of telehealth platforms. Some patients only have front-facing cameras, which won’t work for a virtual exam. Some older patients—though now a very a minor subset of the patient population—don’t have a computer. High-speed internet is not yet available everywhere in the U.S., and mobile phone internet doesn’t always perform as well as home internet service. There remains an unwillingness for IT departments to make the necessary changes to support a telehealth program. And the question of reimbursement still looms as payers haven’t developed a standard to determine how the service is billed.
“All portions of the U.S. are difficult to change, whether due to resistance to technology or a payment system that doesn’t drive innovation,” said Welch. “Telehealth progress is underway and there’s a considerable upside to medication adherence monitoring in drug delivery devices, but we’re still in the very early stages. The question of ‘who pays’ remains, because there are upfront and recurring costs to create connected drug delivery ecosystems. However, we expect to see an increase in medication adherence that will help drive longer term patient outcomes and reduce overall healthcare system costs.”
Telemedicine also involves security risks inherent to the technologies it relies on. The increased demand for telehealth services has created an environment where hackers might try to take advantage of a chaotic situation. Hospitals have made great strides to ensure security in their networks, but individual devices, home patient monitors, and remote-care technologies have no embedded security, making them vulnerable. Further, remote devices lack the network security even a hospital can offer them in a controlled environment. Developing real-time security for IoT devices with increasingly more connectivity is a huge challenge for manufacturers aiming to rapidly deploy.
“All of the patient data is secure and encrypted in all of our systems,” said Dr. Korangy. “We perform routine testing both internally and through third party auditors to ensure the data is secure.”
Any connected device must include cybersecurity strategies in the development plan to provide safeguards against attacks, and this is especially true for telemedicine platforms where a large amount of health data is potentially at risk. Medical and telemedicine professionals must be educated about the new risks and warning signs of a cyberattack.
“We feel very comfortable with the IT security we provide. Our secure telehealth solution was an easy add-on to our Federally secured platform,” said Vetrano. “Cardiac Signals also uses the same secure platform. All of this documentation is on our website. This separates us from many vendors, as it’s a very time-consuming and expensive undertaking for approval.”
Telehealth Beyond the Pandemic
The COVID-19 pandemic has forced much greater adoption of telehealth platforms, but the question remains whether these sweeping changes will continue to any degree once the pandemic has subsided. Over the past two years, Medicare has expanded the ability for clinicians to have brief check-ins with patients through phone, video chat, and online patient portals, known as “virtual check-ins.” Many hope that easier access to telehealth services will be a part of the “new normal” the U.S. is still struggling to reach.
“I think telehealth services will expand,” said Dr. Korangy. “Most medical groups and hospitals that we work with believe this will be the new norm in patient encounters particularly for certain types of encounters. Telehealth and the ability to perform virtual consultations with patients will continue to evolve and become a mainstay for doctor-patient encounters. The same way that outpatient services transformed medical services 20-30 years ago, virtual care is transforming the healthcare delivery model once again. Ultimately the goal is to provide the best possible care to patients in the best possible location in a timely and convenient fashion.”
On March 17, the Trump administration announced it had bolstered access to telehealth services by expanding their Medicare coverage. Beginning on March 6, Medicare is temporary paying clinicians to provide telehealth services for beneficiaries across the U.S. Prior to this, Medicare was only allowed to pay clinicians for telehealth services like routine visits under certain circumstances. The beneficiary had to live in a rural area and travel to a local medical facility to receive services from a doctor in a remote location. The patient was generally not allowed to receive telehealth services in their own home.
Now Medicare beneficiaries can have common office visits, mental health counseling, and preventive health screenings remotely. These services can be offered in any healthcare facility including a physician’s office, hospital, nursing home, rural health clinic, and the home.
“Telehealth was on a slight increase prior to the COVID-19 pandemic, especially in rural America,” said Vetrano. “Value-based care was also on the rise; telehealth is a major part of that. CMS and private insurers made quick adjustments in reimbursement to help hospital and physician practices get reimbursed for telemedicine services as if it was an in-office visit.”
On March 20, the FDA furthered telehealth’s potential by expanding use of devices that measure body temperature, respiratory rate, heart rate, and blood pressure so clinicians can use them remotely for the duration of the pandemic. If healthcare providers can access a patient’s vital signs while the patient is at home, the need for a hospital visit is reduced and the risk of COVID-19 exposure is minimized. The hope is to gradually make this expanded use permanent so patients and clinicians can reap the benefits of remote monitoring for any number of chronic diseases.
“Both hospitals and industry agree what has been adopted very quickly is here to stay,” said Vetrano. “Some research organizations feel we will see upwards of a 50 percent increase in telemedicine over the next two years. Managing patients at home is much more cost-effective. Remote patient monitoring for cardiac and chronic disease patients are in their infancy. These will become a sizable provider segment giving quality patient care at home.”
What was initially meant by CMS and health systems as a bandage to maintain care during the pandemic is beginning to look like the basis for lasting change. If the advancements in telehealth services continue, there could potentially be a re-imagined model of healthcare that aims to meet people wherever they are, physically or otherwise.
“As clinicians and patients learn and become more comfortable with the telehealth approach, we expect longer term usage will increase, and industry data points in this direction,” said Welch. “Roughly 75 percent of hospitals surveyed indicated increased use of telehealth vs. pre COVID-19 levels.1 Post-outbreak, up to 90 percent of hospitals expect greater use of telehealth relative to pre-COVID levels to persist.1”
Future telehealth services might be able to incorporate an ecosystem of technologies that gather and transmit health data like remote monitoring devices, drug delivery technologies, and connected cardiac or neurological implants. Take for example a spinal cord stimulator to treat chronic pain: rather than waiting in agony for an office visit because a particular setting isn’t working to quell a patient’s pain, the patient could quickly conference their doctor who might be able to make the necessary adjustments remotely.
“An end-to-end connected health platform comprised of connected drug delivery devices, apps, and cloud data management will help facilitate improved provider-patient engagement and medication adherence,” said Welch. “We’re contributing to the advancement of telehealth adoption by striving to reduce development time and expense through innovation, efficiency, and low-cost connectivity.”
Reference
“Video telemedicine and virtual patient visits only go so far. Patients with complex cardiovascular diseases will receive incomplete care through just video conference. It’s critical that a provider is able to assess a patient’s heart and lung function remotely,” Eko CEO and co-founder Connor Landgraf told the press. “The Eko intelligent telehealth platform gives providers the most comprehensive picture of a patient’s heart and lung health. Virtual cardiac and pulmonary medicine will become the standard of care even after the pandemic abates.”
Using this technology, providers at hospitals, rural clinics, or nursing homes can stream stethoscope audio and ECG readings to a physician in another room or at a virtual care center, medical center, or specialty clinic. Patients can operate the stethoscope under the supervision of a healthcare provider and use a mobile application to connect via video conference with providers to navigate a self-operated cardiac and pulmonary exam.
Eko Telehealth is one of the latest innovations in telehealth (or telemedicine), the use of medical information exchanged from one site to another via electronic communications to improve a patient’s clinical health status. Telehealth encompasses a rising number of applications and technologies including two-way live or streaming video, videoconferencing, store-and-forward imaging along with the internet, e-mail, smartphones, wireless tools, and other forms of telecommunication. These technologies facilitate leverage of the latest advancements in computer, network, and peripheral medical equipment to promote health. Telehealth is considered to be an integral component of processes that will align with the future of healthcare and improve outcomes in all areas of medicine.
“Innovation in new connected devices and the ability to transmit biometric data in real-time to increase the diagnostic capabilities of the virtual consultations have allowed telehealth capabilities to expand beyond traditional observational consultations,” said S. John Korangy, M.D., founder and CEO of CareClix Inc., an Alexandria, Va.-based provider of software and services for telemedicine and virtual health.
Web Real-Time Communication (WebRTC), a standard to connect two or more users in a private, secure video connection using only a web browser, was designed by Google and open sourced in 2011. Major internet products like Facebook, Google Hangouts, Amazon Kindle, and Slack have used WebRTC technology to build video into applications for customer support or social interaction.
A standard WebRTC application connects two or more users in a Peer-to-Peer (P2P) connection through a Signaling Server custom built for the application. Once the connection is established, the users are connected to each other in a private encrypted connection, allowing them to directly share video, audio, and data with each other. No intermediary servers are required for this, making the connection very secure.
“WebRTC (Web Real-Time Communication)-based solutions built into modern web browsers represent the greatest innovation for telehealth capabilities,” said Jordan Rosen, CEO of Lille Group, an Albany, N.Y.-based provider of healthcare software and technology solutions that improve patient care, reduce costs, and enable healthcare professionals to work most effectively. “Google Chrome has the most complete support; Mozilla Firefox is a very close second. Apple's Safari is significantly behind the other browsers, but the Jitsi community is working hard to close the gap.”
Ease-of-use is of the utmost importance when designing a telehealth platform. The technology has to be accessible to everyone from the most tech-savvy of Millennials to elderly patients that struggle with newer technologies. There must be a simple interface and minimal software installation required to create a platform that can be widely adopted.
“It’s important to first understand the target audience and prioritize the patient experience,” said Charlie Mason, SVP of strategic accounts at Sanmina, a San Jose, Calif.-headquartered global contract manufacturing firm. “If a chronically ill and elderly patient must use a home device to log certain health parameters that are remotely communicated to a doctor, it must be simple and straightforward to use. Highly sophisticated devices may work well in a hospital or doctor’s office, but if they are not intuitive with simple displays, large buttons, and built-in cellular connectivity, they may not be adopted by home users.”
“The portability and durability of a device and an understanding of how it will be used in the home setting, such as in a bathroom or kitchen, are also important considerations to factor into the product development plan,” he added.
“The challenge is to ensure the patient doesn’t have to be a technical guru to join a video call,” said Rosen. “A WebRTC-based solution requires no additional software to install—calls are initiated from the web browser. If you are limited to running Safari, particularly on a smartphone, download the Jitsi Meet app. We delivered a robust telehealth solution in a matter of several days by combining SMS messaging (via Twilio) to invite patients to the virtual appointment with the simplicity of browser-based access.”
Connectivity technology is one of the most efficient ways to gather patient data and offer instructional content for patients, healthcare providers, caregivers, and payers. To use a telehealth platform to increase patient medication adherence and outcomes of therapies, a 360-degree focus must be placed on patients, caregivers, and healthcare providers. A well-functioning, reliable connected health system that embraces all aspects of digital health is necessary to accomplish this.
Partnering with a specialized firm on a connected health system allows collection and analysis of patient data related to diagnosis and medication adherence. Patients can be motivated and instructed on treatment information and medication administration.
“The latest innovations are two-fold: reduced cost and complexity of connectivity and simple sensors, and an increased portion of the population with smartphones and other technologies that facilitate healthcare provider-patient engagement and disease self-management,” said Bill Welch, chief technology officer of Hudson, Wis.-based Phillips-Medisize (a Molex company), a technology-based, global outsource provider of design and manufacturing services, with significant business in the drug delivery, medical device, and primary pharmaceutical packaging markets. “We have designed our low-cost connectivity module to further reduce the cost of creating and manufacturing connected devices by use of a common architecture.”
The COVID-19 pandemic has transformed the delivery of healthcare seemingly overnight. As healthcare institutions attempt to implement social distancing and triage patients, virtual visits with doctors have skyrocketed. According to the Wall Street Journal, CMS telehealth visits surged from 100,000 a week to 300,000 a week as of March 28, and the agency expects this to increase.
"I think the genie's out of the bottle on this one," CMS administrator Seema Verma told Becker’s Hospital Review. "I think it's fair to say that the advent of telehealth has been just completely accelerated, that it’s taken this crisis to push us to a new frontier, but there's absolutely no going back."
Telehealth service providers have rushed to fulfill the sudden need for innovation in their programs the pandemic has created.
“We have been offering our services very much in line with our prior existing programs,” said Dr. Korangy. “We have been adding more laboratory testing partnerships to address the COVID-19 pandemic, as lab testing is a key component.”
“We quickly developed/integrated a telemedicine video conferencing component (Jitsi Meet) to call and access patients within a short time frame for our eScribeHost EHR platform for cardiology users,” added Dennis Vetrano, R.N., director of sales and business development at Lille Group.
Lille Group’s Cardiac Signals cloud-based software solution automatically incorporates transmissions from major cardiac implant device manufacturers (including Medtronic, Boston Scientific, BIOTRONIK, and Abbott Laboratories) into one HHS/CMS certified platform to easily manage a population of patients enrolled in remote monitoring. The platform simplifies management of transmissions while automatically capturing and identifying all billable events.
“We released the Cardiac Signals cloud-based solution to manage remote cardiac implant patients, who need to be remotely monitored. All their transmissions need review by cardiologists or ANP,” said Vetrano. “Cardiology practice ‘Device or Pacer Clinics’ were essentially shut down to most implant patients due to COVID-19—there is a high risk of major complications and morbidity if these patients are infected. Cardiac Signals allows cardiology practices to efficiently manage more device patients and their transmissions, triage appropriately, and capture all billing while providing quality care remotely to Heart Rhythm Society Class I standards.”
Home-based diagnostic testing has become an especially important aspect of telehealth due to the pandemic because patients don’t have to risk exposure from a trip to a testing site to collect a sample. On April 21, the FDA re-issued emergency use authorization for LabCorp’s COVID-19 RT-PCR test to allow testing of samples self-collected by patients at home using the company’s home collection kit. Further, the FDA authorized the first COVID-19 diagnostic test using at-home collection of saliva specimens for emergency use on May 8, to Rutgers Clinical Genomics Laboratory.
“There is a unique opportunity to make home-based testing for infectious diseases more prevalent due to the COVID-19 pandemic and the desire for rapid ongoing testing that can be performed while maintaining social distancing guidelines,” said Mason. “This enabling technology could significantly change how we identify illnesses by reducing the amount of time and number of in-person interactions required to get a diagnosis. If parents suspect their child might be sick with the flu, they could either use a home test system ordered online or pick one up at a pharmacy, avoiding further exposure by visiting a doctor’s office or a lab. We’re currently engaged with a number of companies exploring this business model.”
Connected drug delivery devices are also increasingly being developed to support patient supervision and counseling in the home setting. These advanced devices include features like dosing reminders, adherence trackers, educational tools, and patient diaries to collect patient-reported outcomes. They may also include monitoring tools with interfaces between patients and healthcare professionals.
“There has been significant growth in diagnostics, including devices with the potential for connectivity to track infectious disease data by patient location.,” said Welch. “Our embedded software, hardware design, and electronics manufacturing capabilities are all growing. We support COVID-19 in many categories, from hospital equipment to patient drug delivery devices that allow self-administration vs. going to a healthcare provider for administration. Some of our customers’ innovative drug inhalation devices are also being evaluated for use with direct-to-lung medications to treat COVID-19 respiratory issues.”
Barriers to Adoption
So what’s standing in the way of a proliferation of telehealth services becoming the “new normal”?
“Hospitals have been very slow to upgrade/change their server-based systems to cloud-based systems,” said Vetrano. “The COVID-19 pandemic has sent a loud and clear message to upgrade IT systems to provide quality care, improve efficiency with all staff touching the patient remotely, reduce IT cost and labor, and generate new value-based revenue—especially with chronically ill patients at high risk of serious complications if infected with COVID-19. These patients will need to remain away from the hospital environment unless a clinical intervention is necessary.”
Unfortunately, hospital sluggishness is just one of the many barriers to widespread telehealth adoption. There’s still confusion about what services will and won’t be reimbursed. Costs associated with implementing a telemedicine program can include a great deal of factors like video conferencing adoption and remote monitoring expansion. Healthcare security breaches are on the rise, and patient data can be exposed. Providers may also encounter patient reluctance to engage virtually despite proper broadband and internet resources.
“Connectivity is still an issue in certain parts of the country,” said Dr. Korangy. “Certain patient populations also don’t have the technical capabilities to take full advantage of telehealth.”
A number of other barriers have slowed the widespread adoption of telehealth platforms. Some patients only have front-facing cameras, which won’t work for a virtual exam. Some older patients—though now a very a minor subset of the patient population—don’t have a computer. High-speed internet is not yet available everywhere in the U.S., and mobile phone internet doesn’t always perform as well as home internet service. There remains an unwillingness for IT departments to make the necessary changes to support a telehealth program. And the question of reimbursement still looms as payers haven’t developed a standard to determine how the service is billed.
“All portions of the U.S. are difficult to change, whether due to resistance to technology or a payment system that doesn’t drive innovation,” said Welch. “Telehealth progress is underway and there’s a considerable upside to medication adherence monitoring in drug delivery devices, but we’re still in the very early stages. The question of ‘who pays’ remains, because there are upfront and recurring costs to create connected drug delivery ecosystems. However, we expect to see an increase in medication adherence that will help drive longer term patient outcomes and reduce overall healthcare system costs.”
Telemedicine also involves security risks inherent to the technologies it relies on. The increased demand for telehealth services has created an environment where hackers might try to take advantage of a chaotic situation. Hospitals have made great strides to ensure security in their networks, but individual devices, home patient monitors, and remote-care technologies have no embedded security, making them vulnerable. Further, remote devices lack the network security even a hospital can offer them in a controlled environment. Developing real-time security for IoT devices with increasingly more connectivity is a huge challenge for manufacturers aiming to rapidly deploy.
“All of the patient data is secure and encrypted in all of our systems,” said Dr. Korangy. “We perform routine testing both internally and through third party auditors to ensure the data is secure.”
Any connected device must include cybersecurity strategies in the development plan to provide safeguards against attacks, and this is especially true for telemedicine platforms where a large amount of health data is potentially at risk. Medical and telemedicine professionals must be educated about the new risks and warning signs of a cyberattack.
“We feel very comfortable with the IT security we provide. Our secure telehealth solution was an easy add-on to our Federally secured platform,” said Vetrano. “Cardiac Signals also uses the same secure platform. All of this documentation is on our website. This separates us from many vendors, as it’s a very time-consuming and expensive undertaking for approval.”
Telehealth Beyond the Pandemic
The COVID-19 pandemic has forced much greater adoption of telehealth platforms, but the question remains whether these sweeping changes will continue to any degree once the pandemic has subsided. Over the past two years, Medicare has expanded the ability for clinicians to have brief check-ins with patients through phone, video chat, and online patient portals, known as “virtual check-ins.” Many hope that easier access to telehealth services will be a part of the “new normal” the U.S. is still struggling to reach.
“I think telehealth services will expand,” said Dr. Korangy. “Most medical groups and hospitals that we work with believe this will be the new norm in patient encounters particularly for certain types of encounters. Telehealth and the ability to perform virtual consultations with patients will continue to evolve and become a mainstay for doctor-patient encounters. The same way that outpatient services transformed medical services 20-30 years ago, virtual care is transforming the healthcare delivery model once again. Ultimately the goal is to provide the best possible care to patients in the best possible location in a timely and convenient fashion.”
On March 17, the Trump administration announced it had bolstered access to telehealth services by expanding their Medicare coverage. Beginning on March 6, Medicare is temporary paying clinicians to provide telehealth services for beneficiaries across the U.S. Prior to this, Medicare was only allowed to pay clinicians for telehealth services like routine visits under certain circumstances. The beneficiary had to live in a rural area and travel to a local medical facility to receive services from a doctor in a remote location. The patient was generally not allowed to receive telehealth services in their own home.
Now Medicare beneficiaries can have common office visits, mental health counseling, and preventive health screenings remotely. These services can be offered in any healthcare facility including a physician’s office, hospital, nursing home, rural health clinic, and the home.
“Telehealth was on a slight increase prior to the COVID-19 pandemic, especially in rural America,” said Vetrano. “Value-based care was also on the rise; telehealth is a major part of that. CMS and private insurers made quick adjustments in reimbursement to help hospital and physician practices get reimbursed for telemedicine services as if it was an in-office visit.”
On March 20, the FDA furthered telehealth’s potential by expanding use of devices that measure body temperature, respiratory rate, heart rate, and blood pressure so clinicians can use them remotely for the duration of the pandemic. If healthcare providers can access a patient’s vital signs while the patient is at home, the need for a hospital visit is reduced and the risk of COVID-19 exposure is minimized. The hope is to gradually make this expanded use permanent so patients and clinicians can reap the benefits of remote monitoring for any number of chronic diseases.
“Both hospitals and industry agree what has been adopted very quickly is here to stay,” said Vetrano. “Some research organizations feel we will see upwards of a 50 percent increase in telemedicine over the next two years. Managing patients at home is much more cost-effective. Remote patient monitoring for cardiac and chronic disease patients are in their infancy. These will become a sizable provider segment giving quality patient care at home.”
What was initially meant by CMS and health systems as a bandage to maintain care during the pandemic is beginning to look like the basis for lasting change. If the advancements in telehealth services continue, there could potentially be a re-imagined model of healthcare that aims to meet people wherever they are, physically or otherwise.
“As clinicians and patients learn and become more comfortable with the telehealth approach, we expect longer term usage will increase, and industry data points in this direction,” said Welch. “Roughly 75 percent of hospitals surveyed indicated increased use of telehealth vs. pre COVID-19 levels.1 Post-outbreak, up to 90 percent of hospitals expect greater use of telehealth relative to pre-COVID levels to persist.1”
Future telehealth services might be able to incorporate an ecosystem of technologies that gather and transmit health data like remote monitoring devices, drug delivery technologies, and connected cardiac or neurological implants. Take for example a spinal cord stimulator to treat chronic pain: rather than waiting in agony for an office visit because a particular setting isn’t working to quell a patient’s pain, the patient could quickly conference their doctor who might be able to make the necessary adjustments remotely.
“An end-to-end connected health platform comprised of connected drug delivery devices, apps, and cloud data management will help facilitate improved provider-patient engagement and medication adherence,” said Welch. “We’re contributing to the advancement of telehealth adoption by striving to reduce development time and expense through innovation, efficiency, and low-cost connectivity.”
Reference